The Complexity of Co-occurring Disorders
Dealing with co-occurring disorders isn’t just about juggling two separate issues—it’s about understanding how deeply intertwined mental health disorders and substance use disorders (SUD) can be. These dual diagnoses require an approach that is as multifaceted as the conditions themselves. It’s not simply a matter of treating one problem while ignoring the other; both need addressing concurrently to achieve effective management and recovery.
Co-occurring disorders, or dual diagnosis, refer to the simultaneous presence of a mental health disorder alongside a substance use disorder. The prevalence of these intertwined conditions necessitates a nuanced and multifaceted approach to treatment and support. Studies have shown that people with mental health disorders are more likely to experience substance dependence compared to those without mental health issues. This intersection highlights the need for integrated care that addresses both conditions simultaneously.
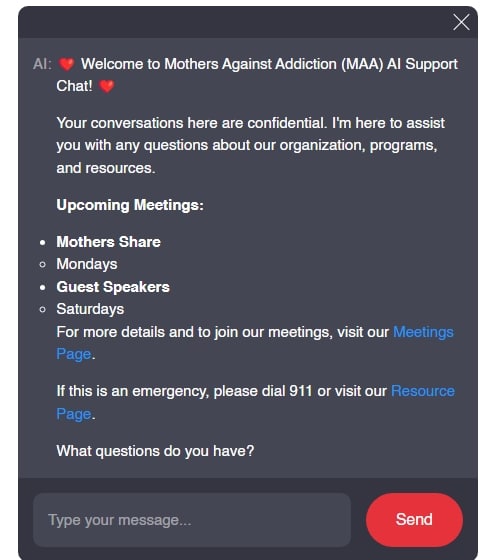
Understanding this complexity, along with the associated risks, is crucial for effective intervention and support—particularly for families struggling to navigate these challenging waters. At Mothers Against Addiction, we strive to light the path for parents who are supporting a child through these daunting struggles or grappling with the unimaginable loss due to addiction.
Common Co-Occurring Disorders: Notable Examples in Recent Years
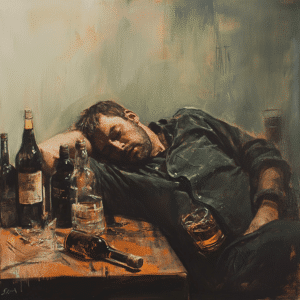
Depression and Alcohol Abuse
A recurrent example of co-occurring disorders is the link between depression and alcohol abuse. In fact, a 2022 report by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) indicated that over 30% of individuals suffering from major depression also engage in significant alcohol consumption. This comorbidity can trap individuals in a vicious cycle—where depression leads to increased alcohol use, which in turn deepens depressive symptoms. This dual challenge makes it exceptionally difficult to address either condition in isolation.
Anxiety Disorders and Prescription Drug Dependence
Anxiety disorders, such as generalized anxiety disorder (GAD), frequently coexist with prescription drug dependence. The misuse of benzodiazepines like Xanax and Valium has particularly risen. In 2023, the American Psychological Association (APA) reported that approximately 20% of individuals with GAD were misusing prescription medications. High-profile cases, such as that of Demi Lovato, have brought public attention to these struggles, underlining the dual nature of these battles and the importance of comprehensive treatment plans.
| Aspect | Details |
| Definition | Co-occurring disorders refer to the coexistence of both a mental illness and a substance use disorder (SUD), also known as dual diagnosis. |
| Common Pairings | – Alcohol addiction and depression. – Schizophrenia and substance use disorder. – Anxiety disorder and drug addiction. – Intellectual or learning disability and mental illness. |
| Prevalence | People with mental illness are more likely to experience an SUD than those without a mental illness. Adults with dual diagnosis constitute 25.8% of those with any psychiatric disorder and 36.5% of those with any SUD. |
| Risk Factors | – Genetics: Both conditions can run in families. – Environmental Factors: Stress and trauma can contribute to the onset of both conditions. |
| Common Symptoms | – Social withdrawal. – Appetite or weight changes. – Angry, violent, or reckless behavior. |
| Characteristics of Individuals | People with co-occurring disorders may use alcohol and other drugs episodically or continuously to reduce symptoms of their illness or the side effects of their medication. |
| Treatment Approach | The most effective treatment is an integrated approach that concurrently addresses both the mental health issue and the substance use issue, typically using cognitive behavioral therapy to enhance interpersonal and coping skills. |
| Therapeutic Strategies | – Cognitive Behavioral Therapy (CBT) for boosting interpersonal and coping skills. – Motivational approaches to support functional recovery. |
| Terminology | “Dual Diagnosis” refers to treatment for those with both a mental illness and an addiction. “Co-occurring disorders” is another term frequently used to describe the simultaneous presence of both conditions. |
| Impact and Worsening Effect | If not addressed, co-occurring disorders may exacerbate each other. For example, depression can worsen alcoholism and vice versa. |
| Integrated Care | Integrated treatment is recommended, where both conditions are treated simultaneously by the same provider or team, to improve outcomes and address the complex interactions between the disorders. |
The Risks and Impact of Dual Diagnosis
Physical Health Complications
Individuals facing co-occurring disorders often endure significant physical health challenges. Mental health symptoms coupled with substance abuse can exacerbate chronic illnesses, weaken immune systems, and lead to premature death. A notable 2023 study in “The Lancet Psychiatry” highlighted a stark reality: patients with dual diagnoses had a life expectancy reduction of up to 15 years compared to the general population. The physical toll of these intertwined conditions cannot be underestimated, necessitating an urgent and comprehensive approach to treatment.
Social and Economic Consequences
The social and economic impact of co-occurring disorders extends far beyond the individual. Families often bear significant emotional and financial burdens due to treatment costs and lost productivity. Harvard’s 2024 economic impact study estimated that dual diagnoses cost the U.S. economy approximately $140 billion annually in healthcare expenses and lost workforce participation. These figures underscore the need for systemic support and resources not just for individuals, but for their families and broader communities as well.
Innovative Treatment Approaches for Co-occurring Disorders
Integrated Treatment Models
One of the most promising developments in addressing co-occurring disorders is the rise of integrated treatment models. These programs tackle both mental health and substance use disorders simultaneously. Assertive Community Treatment (ACT) and the Collaborative Care Model have shown particularly effective results. A 2023 review in the “Journal of Substance Abuse Treatment” highlighted that patients receiving integrated care were twice as likely to remain sober and symptom-free compared to those undergoing separate treatments.
Role of Peer Support and Community-Based Programs
Peer-led initiatives and community-based programs are vital in supporting individuals with dual diagnoses. Organizations such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) have adapted their programs to better address co-occurring mental health issues. Non-profits like the National Alliance on Mental Illness (NAMI) are providing crucial education and peer support, empowering individuals to maintain long-term recovery. These community-based efforts create a supportive environment that fosters resilience and continuous improvement.
Preventative Measures and Early Intervention
Education and Awareness Campaigns
Raising awareness about the risks and signs of co-occurring disorders is crucial for early intervention. In 2024, the Substance Abuse and Mental Health Services Administration (SAMHSA) launched a national campaign emphasizing the importance of recognizing early symptoms and seeking timely help. These educational campaigns aim to reduce stigma, encourage open conversations about mental health and substance dependence, and promote proactive care.
Screening and Early Identification
Early identification through routine screenings in primary care settings can significantly enhance intervention outcomes. According to the 2023 guidelines from the American Medical Association (AMA), annual screenings for high-risk individuals are recommended to enable timely and integrated treatment approaches. These screenings can help in identifying potential co-occurring disorders before they become deeply entrenched, allowing for more effective and holistic care.
Reflect and Reinforce: Towards a Supportive Future
Understanding co-occurring disorders and the dual diagnosis risks they carry is key to fostering a comprehensive approach to treatment and recovery. Through persistent education, innovative treatment models, and robust community support, we can build a more empathetic and effective landscape for managing these intertwined conditions. By sharing success stories of individuals who have triumphed over dual diagnoses, we’re reminded that recovery is possible with the right blend of support, awareness, and intervention.
As we move forward, it’s imperative to refine our strategies, advocate for inclusive healthcare policies, and foster environments where individuals can seek help without shame or fear. At Mothers Against Addiction, we stand by you—offering understanding, resources, and a community dedicated to turning the tide against the challenges posed by co-occurring disorders. Supporting one another, we can make meaningful strides in helping those we love lead healthier, fuller lives.
For more information on substance dependence, withdrawal Symptoms, and specific support For Mothers, visit Mothers Against Addiction.
Embrace this resource-rich article, bookmark it, share it, and remember, you are not alone. Our combined resilience, compassion, and proactive efforts will pave the way for more successful recoveries and supportive communities.
Co-occurring Disorders: Dual Diagnosis Risks
Understanding Co-Occurring Disorders
Navigating life with co-occurring disorders can be like trying to juggle flaming torches while riding a unicycle. Did you know that individuals with a dual diagnosis often face more significant challenges because they’re dealing with both a mental health disorder and substance addiction simultaneously? It’s like trying to stay on top of your bills during the Ups Holidays 2024 season. The complexity of handling these disorders together can be overwhelming, making early diagnosis and comprehensive treatment essential.
Surprising Trivia and Interesting Facts
Here’s a fascinating tidbit: Nearly half of the people with a severe mental disorder are also affected by substance abuse. Imagine if you’re a fan of DeAndre Hopkins, Ravens’ star receiver, juggling both intense training and a chronic illness. It’s a herculean task requiring immense support and perseverance. Understanding that mental health and substance abuse can amplify each other gives us insight into why holistic and integrated treatment approaches are necessary.
A Mosaic of Challenges
Relapse rates for those with dual diagnoses are significantly higher. This is similar to how you have to intricately figure out How To calculate capital Gains tax—you need precision and clear guidance, or you’re bound to encounter setbacks. For families and caregivers, it’s crucial to educate themselves on these intertwined issues, often realizing that one condition doesn’t simply cause the other; they perpetuate a vicious cycle, much like the never-ending chapters of Minato Manga.
Fun Facts with a Meaningful Impact
Let’s sprinkle in a little more trivia, shall we? Did you know that certain behavioral therapies can be more effective for those with co-occurring disorders than standard treatments? It adds a layer of optimism, much like an unexpectedly delightful burst of flavor in a dish—Mmmmmm! This underscores the significance of innovative and individualized treatment programs, tailored to address both the mental health and substance use aspects simultaneously.
Understanding these complexities and the need for integrative care can help improve outcomes for individuals grappling with dual diagnoses. The path may be tough, but with the right help, a brighter future is just a step away.
What is an example of a co-occurring disorder?
An example of a co-occurring disorder is when someone struggles with alcohol addiction and depression at the same time. Both issues need attention and treatment simultaneously to help the person recover.
What is a co occurrence of disorders?
Co-occurrence of disorders refers to a situation where an individual has both a mental illness and a substance use disorder, such as anxiety and drug addiction. These conditions often interact and intensify each other.
How are co-occurring mental disorders treated?
Co-occurring mental disorders are best treated using an integrated approach, which combines cognitive behavioral therapy to improve coping skills and motivation, along with simultaneous treatment for both the mental health issue and the substance use disorder.
What is the difference between dual diagnosis and co-occurring disorders?
Dual diagnosis and co-occurring disorders essentially refer to the same concept, where a person has both a mental illness and a substance use disorder. Dual diagnosis is the term most often used in treatment contexts.
Is ADHD a co-occurring disorder?
Attention Deficit Hyperactivity Disorder (ADHD) can be a co-occurring disorder, particularly when it exists alongside another condition such as anxiety or substance use disorder.
Is PTSD a co-occurring disorder?
Post-Traumatic Stress Disorder (PTSD) is indeed a co-occurring disorder, as it often accompanies substance use disorders or other mental illnesses like depression or anxiety.
What is another name for a co-occurring disorder?
Another name for a co-occurring disorder is dual diagnosis, which refers to the presence of both a mental health condition and a substance use disorder in the same individual.
Why do co-occurring disorders happen?
Co-occurring disorders often happen because mental health disorders and substance use disorders can share common risk factors, such as genetics, environmental influences, and stress, making it more likely for an individual to develop both.
What are co-occurring disorders and autism?
Co-occurring disorders and autism can coexist, where an individual with an autism spectrum disorder also has another mental health condition, such as anxiety or depression, along with a substance use disorder.
Which best describes co-occurring disorders?
Co-occurring disorders are best described as the simultaneous presence of a mental illness and a substance use disorder, where each condition can influence and worsen the other.
What is having two coexisting psychological disorders called?
Having two coexisting psychological disorders is called a dual diagnosis, which means dealing with both a mental health issue and a substance use disorder at the same time.
Can personality disorders co-occur?
Yes, personality disorders can co-occur with other mental health conditions or substance use disorders, often making treatment more complex and requiring integrated approaches.
What are the three most common co-occurring disorders?
The three most common co-occurring disorders include alcohol addiction and depression, schizophrenia and substance use disorder, and anxiety disorder and drug addiction.
Can you have two mental illnesses at the same time?
Yes, you can have two mental illnesses at the same time, such as depression and anxiety, which can complicate diagnosis and treatment but are often interconnected.
What’s the difference between comorbidity and co-occurring?
Comorbidity and co-occurring both describe the presence of more than one disorder in the same person; however, comorbidity more broadly refers to any coexisting conditions, while co-occurring specifically refers to mental health and substance use disorders.
Which best describes co-occurring disorders?
Co-occurring disorders best describe situations where a person has both a substance use disorder and a mental health condition, like drug addiction and schizophrenia, impacting each other.
What is the best example of dual diagnosis?
The best example of dual diagnosis is someone dealing with both depression and alcoholism, where each condition may exacerbate the other and require comprehensive treatment.
Is OCD a co-occurring disorder?
Obsessive-Compulsive Disorder (OCD) can be a co-occurring disorder, particularly if it exists alongside substance use disorders or other mental health issues like anxiety or depression.
What is the co-occurrence of two disorders in the same individual?
The co-occurrence of two disorders in the same individual typically refers to having both a mental health disorder and a substance use disorder, such as bipolar disorder and drug addiction happening simultaneously.