Dual diagnosis—also known as co-occurring disorders—hits at the heart of a complex issue where mental health disorders and substance use disorders (SUD) coexist in an individual. This convoluted interplay demands a nuanced approach to identification and treatment, having both compassion and resilience. Here at www.MothersAgainstAddiction.org, we understand the trials and tribulations parents face when their child grapples with these intertwined battles, or tragically, when they lose a child to this double-edged sword.
Understanding Dual Diagnosis: What It Entails
Dual diagnosis entails the presence of both a mental health disorder and a substance use disorder simultaneously. Common scenarios include battling depression and alcoholism or dealing with anxiety while misusing prescription drugs. Without balanced treatment, these conditions can exacerbate one another, creating a vicious cycle that’s hard to break.
The importance of treating both disorders concurrently cannot be overstated. The bygone era of isolating mental health treatments from addiction services is over; current thinking emphasizes that comprehensive care is the gold standard. Recognizing the intertwined nature of these disorders helps to forge a path towards genuine recovery.
The Prevalence of Dual Diagnosis in Today’s Society
Shockingly, the National Institute on Drug Abuse (NIDA) reports that approximately 7.9 million adults in the U.S. live with co-occurring disorders. These statistics underscore the urgency for tailored treatment protocols and more resources to address this burgeoning issue. The prevalence data also sheds light on the extensive impact of dual diagnosis on our communities and families, prompting a call for more specialized care strategies.
| Aspect | Details |
| Definition | Dual diagnosis, also known as co-occurring disorders or comorbidity, refers to the concurrent presence of a mental disorder and a substance use disorder (SUD). |
| Other Names | Co-occurring disorders, comorbidity. |
| Examples | Depression and alcoholism, anxiety and prescription drug misuse. |
| Prevalence | Common occurrence; many individuals with a mental illness also have a substance use disorder. |
| Causes | Factors may include genetic predisposition, environmental stressors, trauma, or self-medication for mental health symptoms. |
| Characteristics | Continuous or episodic use of substances to alleviate psychological symptoms or side effects of medication. |
| Assessment | Involves thorough evaluation, including both substance abuse and mental health assessments to determine severity and underlying causes. |
| Best Treatment Method | Integrated intervention, where both mental illness and substance abuse are treated simultaneously. |
| Outdated Practice | The approach of “I cannot treat your depression because you are also drinking” is outdated. |
| Treatment Goals | Alleviate symptoms of both disorders, improve functioning, and enhance quality of life. |
| Challenges | Difficulty in diagnosis due to overlapping symptoms, stigma attached to both mental illness and substance use disorders, and the need for comprehensive care plans. |
| Key Components | Collaboration between mental health professionals and addiction specialists, individualized treatment plans, ongoing support, and therapy. |
| Importance of Treatment | Without addressing both conditions, each disorder may exacerbate the other, leading to a decline in overall mental and physical health. |
Common Mental Health Disorders in Dual Diagnosis Cases
Depression and Substance Abuse
People often turn to substances like alcohol or opioids as a way to handle the symptoms of depression. Sadly, while the temporary relief may seem like an escape, it ultimately exacerbates both the depression and the substance abuse disorder. Parents particularly grapple with the agonizing dilemma of witnessing their children spiral down this dark path.
Anxiety Disorders and Alcoholism
For some, a drink may temporarily mute the sharp edges of anxiety, but it’s a double-edged sword. Eventually, the reliance on alcohol can deepen both the anxiety and the addiction, creating a cycle that feels impossible to escape. This dual struggle can be particularly heartbreaking for parents to watch.
Post-Traumatic Stress Disorder (PTSD) and Drug Addiction
PTSD, often linked with veterans and trauma survivors, can lead individuals down the path of drug misuse as a coping mechanism. This self-medication might offer a fleeting reprieve but tends to worsen the PTSD symptoms over time. Knowing that their child’s suffering is spiraling into addiction is an unbearable cross for any parent to bear.
Treatment Approaches for Dual Diagnosis
Integrated Treatment Programs
Integrated treatment programs are the gold standard for addressing dual diagnosis. Prestigious facilities like the Hazelden Betty Ford Foundation and Johns Hopkins Medicine offer comprehensive plans combining psychotherapy, medication management, and peer support.
Cognitive-Behavioral Therapy (CBT)
Cognitive-behavioral therapy (CBT) shines as a highly effective method for treating co-occurring disorders. It equips individuals with the tools needed to manage negative thought patterns and behaviors, playing a vital role in mental health recovery and addiction treatment.
Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) employs FDA-approved medications to manage withdrawal symptoms and psychological cravings. Suboxone and Naltrexone are frequently used, particularly effective for opioid and alcohol use disorders.
Success Stories: Real-Life Examples
Robert Downey Jr.
Robert Downey Jr.’s well-documented struggle with addiction and bipolar disorder offers a beacon of hope. His transparent journey and eventual recovery illustrate the power of integrated treatment and the resilience to overcome dual diagnosis.
Demi Lovato
Singer and actress Demi Lovato’s candid discussion about her battles with bipolar disorder and substance abuse brings a message of hope and resilience. Her ongoing recovery, bolstered by proper treatment, provides a tangible example for others facing similar obstacles.
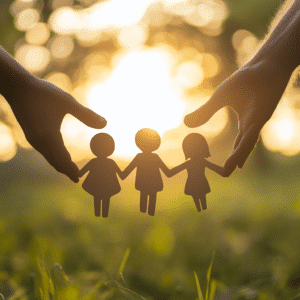
The Importance of Support Networks
Family support is crucial in the recovery journey. Organizations such as Mothers Against Addiction and Al-Anon provide vital emotional and practical assistance. The invaluable role of these support networks cannot be overstated, as they offer a lifeline for families dealing with dual diagnosis challenges.
Challenges and Misconceptions in Treating Dual Diagnosis
Stigma Surrounding Mental Illness and Addiction
Both mental illness and addiction are fraught with stigma. Overcoming this stigma is imperative to create a supportive environment where individuals feel safe seeking help without judgment.
Coordination of Care
Effective coordination between mental health professionals and addiction specialists is paramount for successful treatment of dual diagnosis. Yet, systemic fragmentation in healthcare presents a significant hurdle, making seamless care transitions and collaboration essential.
Innovative Strategies for the Future
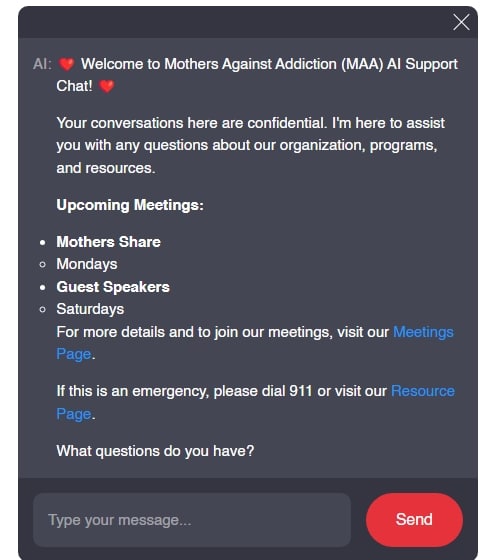
The future of dual diagnosis treatment is bright, thanks to technological advancements and personalized care strategies. Innovations like teletherapy and AI-driven personalized treatment plans are revolutionizing how we manage co-occurring disorders.
A Holistic Future for Dual Diagnosis Care
By weaving together personalized care, enhancing public awareness, and leveraging technological advancements, we can pave the way for more effective management of dual diagnosis. At www.MothersAgainstAddiction.org, we are committed to shining a light on these challenges and supporting a healthier future for families affected by dual diagnosis.
Together, we can take one step closer to a world where the duality of such complex issues is met with compassion, resilience, and effective treatment. Let’s foster a brighter, healthier future for everyone grappling with these intertwined battles.
Remember, you’re not alone. There’s hope, there’s help, and together, we can tackle dual diagnosis head-on.
Dual Diagnosis: Addressing Co-Occurring Disorders
What is Dual Diagnosis?
Dual diagnosis, or co-occurring disorders, refers to someone who struggles with both a mental health issue and addiction. Fascinatingly, many people living in a tiny house on Wheels have reported that the shift to minimalist living has helped manage their dual diagnosis. This trend underscores the importance of creating a stable environment when facing these challenges, a topic often addressed in discussions around Mental health And Addiction.
The Link Between Anxiety and Addiction
It’s interesting to note that anxiety and addiction go hand-in-hand more often than you might think. No wonder why places like the dispensary in Baltimore have begun to cater to those seeking relief from both conditions. Furthermore, stress and anxiety can sometimes trigger the need to escape via substances, highlighting the significance of timely intervention and supportive environments. Fun fact: while Joe Bonsall of the Oak Ridge Boys might be famous for his music, he’s also an advocate for mental health awareness.
Depression and Addiction
On a similar note, Depression and addiction are another common duo. It’s startling but true that depression can amplify the desire for substance use, and vice versa. Addressing these intertwined issues is crucial for effective treatment. For instance, assembling something fun like the re-ment Nintendo Kirby’s kitchen mini figure set blind box can serve as a therapeutic activity, providing a small but meaningful distraction from the strains of daily life.
Surprising Stats and Solutions
Did you know that securing the right home loan can have a significant impact on someone dealing with dual diagnosis? Establishing a stable living situation provides a cornerstone for recovery. Much like a tiny house on wheels, having a secure space can reduce stress and alcohol or substance use, fostering a healthier lifestyle.
When it comes to tackling dual diagnosis, comprehensive care is paramount. Combining mental health treatment with addiction therapy offers a more holistic approach, addressing both sides of the coin to pave a path to recovery.
What does dual diagnosis mean?
Dual diagnosis means having both a mental illness and a substance use disorder at the same time, such as struggling with depression and alcoholism.
What is the best example of dual diagnosis?
A good example of dual diagnosis is someone who suffers from anxiety while misusing prescription drugs.
What is the new term for dual diagnosis?
Dual diagnosis is now often referred to as co-occurring disorder or comorbidity.
Is there a cure for dual diagnosis?
There isn’t a straightforward cure for dual diagnosis, but with integrated treatment, both conditions can be managed effectively.
What are the risks of dual diagnosis?
The risks of dual diagnosis include worsening of both mental health and substance use issues, making treatment more complicated.
What is dual diagnosis for ADHD?
For someone with ADHD, dual diagnosis could mean dealing with both the symptoms of ADHD and substance abuse, like using drugs to cope with hyperactivity.
How common is dual diagnosis?
Dual diagnosis is pretty common as many people with mental health issues also struggle with substance abuse.
What is another word for dual diagnosis?
Another word for dual diagnosis is co-occurring disorder.
What is the challenge of dual diagnosis?
The challenge of dual diagnosis lies in the need to treat both mental health and substance abuse issues simultaneously, which can be complex.
What are the most common mental health disorders?
The most common mental health disorders include depression, anxiety, bipolar disorder, and schizophrenia.
Can you have two mental illnesses at the same time?
Yes, it’s possible to have more than one mental illness at the same time, like depression and anxiety.
What is the difference between a co-occurring disorder and a dual diagnosis?
There’s no difference between co-occurring disorder and dual diagnosis; they both mean having a mental illness and a substance use disorder simultaneously.
What drugs cause personality changes?
Substances like alcohol, methamphetamine, and opioids can cause significant personality changes.
How rare is dual personality disorder?
Dual personality disorder, or Dissociative Identity Disorder, is very rare and different from dual diagnosis.
What is the stigma of dual diagnosis?
The stigma of dual diagnosis involves misconceptions and negative attitudes about people who have both mental health and substance use disorders, which can lead to judgment and discrimination.
What is the difference between a dual diagnosis and co-occurring disorder?
The terms dual diagnosis and co-occurring disorder are interchangeable and mean the same thing.
What is the role of the nurse in dual diagnosis?
Nurses play a crucial role in dual diagnosis treatment by providing medical care, support, and education to help manage both mental health and substance use problems.
How does a dual diagnosis affect the family?
Having a family member with a dual diagnosis can be very challenging, leading to emotional stress, financial strain, and the need for additional support.
What is the stigma of dual diagnosis?
The stigma of dual diagnosis involves facing judgment and lack of understanding from others, making it harder for individuals to seek or receive proper treatment.