The interplay between depression and addiction forms a complex and often concealed challenge faced by many individuals and their families. This critical connection underlies the struggle of numerous patients and poses intricate problems that demand detailed examination and understanding. At Mothers Against Addiction, we recognize the heavy load parents carry and strive to offer supportive resources.
Recognizing the Dual Struggle: Depression and Addiction
Understanding the simultaneous occurrence of depression and addiction is the first step towards comprehensive mental health support. Depression and addiction often go hand-in-hand, and recognizing this dual struggle is key to providing effective help.
Biochemical Basis
Recent studies have shown that depression and addiction share common neurological pathways. Both disorders significantly impact the brain’s reward system. For instance, depression and addiction involve disruptions in dopamine, a neurotransmitter responsible for pleasure and motivation. When the balance of dopamine is disturbed, it creates a vicious cycle of substance abuse in an attempt to alleviate depressive symptoms, ultimately making matters worse.
Psychological Factors
Depression often leads individuals to use substances as a form of self-medication. However, this temporary relief comes at a high price – the development of substance dependence. The psychological links between depression and addiction include patterns like learned helplessness and conditioned reinforcement. When you’re stuck in such a cycle, it feels like there’s no way out, but understanding these patterns is the first step to breaking free.
Social Influences and Case Studies
The social catalysts of depression and addiction cannot be ignored. Stigma, social isolation, and family dynamics play significant roles. Renowned individuals like David Foster Wallace and Chris Cornell struggled with both conditions, highlighting the powerful influence of societal factors. Understanding these influences through such cases offers valuable insights into prevention and treatment.
Symptoms: Identifying Co-occurring Disorders
Identifying the signs and symptoms of co-occurring depression and addiction can be an arduous task due to their intertwined nature. Expert analyses from clinical psychologists, such as Dr. Lisa Najavits, offer critical guidance on differential diagnosis techniques.
Common Symptoms
- Persistent Sadness & Substance Use: Persistent sadness is a hallmark of depression. When coupled with an increasing reliance on substances like alcohol or opioids, it points towards a co-occurring disorder.
- Changes in Sleep and Appetite: Depression can lead to insomnia or hypersomnia. Substance use further disrupts natural sleep and eating patterns, adding another layer of complexity.
Behavioral Red Flags
Behavioral shifts are critical indicators. Individuals may withdraw from social obligations or display erratic behaviors. Recognizing these red flags early can prevent the progression from mild substance abuse to severe addiction. Studies have shown that timely interventions can make a huge difference.
| Aspect | Description |
| Commonality | Depression is widespread among individuals battling substance abuse. |
| Trigger/Intensifier | Substance abuse can provoke or worsen feelings of loneliness, sadness, and hopelessness operative in depression. |
| Dual Diagnosis Statistics | Approximately one-third of people with major depression also have an alcohol problem. |
| Impact on Family Life | Caring for someone with depression can strain relationships and create family tension. |
| Findings Support | Joining support groups and talking to others in similar situations may provide relief and coping strategies. |
| Cognitive Symptoms | Difficulty concentrating, remembering, or making decisions. |
| Sleep Disturbances | Difficulty sleeping, waking too early, or oversleeping. |
| Appetite Changes | Varying appetite or unintended weight changes. |
| Physical Symptoms | Persistent physical aches, headaches, cramps, or digestive issues without clear physical causes. |
| Duration of Episodes | Depressive episodes typically last most of the day, nearly every day, for at least two weeks. |
| Emotional & Psychological Symptoms | Low self-worth, thoughts about dying, hopelessness about the future, tiredness, and poor concentration. |
Case Scenarios: Interventions That Worked
Real-world examples provide practical insights into effective intervention strategies.
Sarah’s Story: A Holistic Approach
Sarah, a 26-year-old struggling with depression and alcohol dependence, found success through a Dual-diagnosis treatment facility. Her treatment combined cognitive-behavioral therapy (CBT) with a twelve-step program, and included family counseling sessions. This holistic approach led to sustained recovery, proving that comprehensive strategies work.
Pediatric Dual-Diagnosis: The Jackson Youth Program
The Jackson Youth Program in Seattle specializes in adolescent mental health And addiction treatment. Their integrated approach, involving school support and peer-led group therapy, has yielded significant success rates over the past five years. It underscores the importance of age-appropriate interventions to combat Depression and addiction.
Prevention: Early and Effective Strategies
Exploring preemptive measures can reduce the incidence of depression and addiction.
School-Based Programs
Initiatives like the LifeSkills Training Program aim to equip students with coping mechanisms for stress and peer pressure. Research shows that such programs reduce the onset of substance use and encourage help-seeking behavior for depressive symptoms. Implementing these strategies early can make a substantial difference.
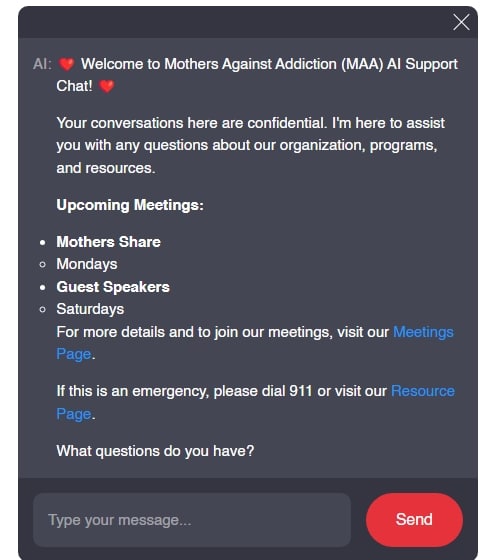
Community Outreach and Support Groups
Local community programs like Alcoholics Anonymous (AA) and the Depression and Bipolar Support Alliance (DBSA) offer valuable resources for both prevention and recovery. Engaging in these communities reduces the isolation often felt by those struggling with depression and addiction.
Innovative Approaches and Future Directions
Research is continually advancing towards more effective treatments for co-occurring depression and addiction.
Technological Advances in Treatment
Telehealth services and mobile applications like Woebot are expanding access to mental health resources, providing immediate support and tracking treatment progress. These technological innovations make it easier for people to access care when they need it most.
Pharmacological Interventions
Emerging medications, such as ketamine for treatment-resistant depression and drugs like naltrexone and buprenorphine for opioid addiction, show promise in providing dual relief from depression and substance dependence. The future looks brighter with these developments on the horizon.
Path Forward: Creating Hope and Resilience
The battle against depression and addiction calls for continued advocacy, education, and research. By deepening our understanding and implementing comprehensive strategies, we pave the way for resilient recovery narratives and a society better equipped to support those in need. At Mothers Against Addiction, we strive to transform hidden struggles into stories of hope and recovery, fostering communities of empathy and evidence-based intervention. Let’s work together to bring light to those battling depression and addiction, creating a better future for all.
For more detailed information on Mental Health and Addiction, visit our site here.
Depression and Addiction: Hidden Struggles
Depression and addiction can coexist like unwelcome houseguests, each feeding off the other’s intensity. Did you know that these challenges aren’t just about enduring tough days but also understanding hidden struggles? For instance, anxiety often plays a significant role in addiction-related issues. You might find similarities among those battling both, revealing the tangled web of emotions and triggers. Check out this resource on the connection between anxiety And addiction to dive deeper.
Fun Facts & Trivia
Ever heard the phrase “that’s cap”? It essentially means “that’s a lie” or “falsehood,” which aligns perfectly with the deceitful nature of depression and addiction. People suffering from these conditions often put on brave faces, masking the pain underneath—an internal “cap” hiding their real struggles. Understanding this is vital because the societal stigma attached to both conditions can exacerbate the situation. To expand your slang vocabulary, here’s an overview of “that’s cap” meaning.
Hidden Struggles & Quirky Facts
Depression and addiction often cause individuals to seek solace in unorthodox places. For instance, someone struggling with these issues in Baltimore might look up the best dispensary near them for temporary relief. Yet, while some may find momentary peace, it’s crucial to understand that such solutions can be a slippery slope, often leading to deeper issues if not managed correctly. Curiously, the need for immediate remedies sheds light on why understanding the root cause is imperative.
Incidentally, would you believe that some video game characters resonate strongly with these themes? Take Kokichi Oma, a character from a popular game series, for example. His intricate and dual-faced nature mirrors the deceptive calm that hides deeper struggles. Characters like Kokichi Oma bring to the forefront how even within entertainment, underlying themes of mental health struggles are subtly yet effectively portrayed, making it easier to discuss these issues.
It’s not surprising that tackling both depression and addiction often requires long-term planning and support. Interestingly, think about how people approach significant commitments like a 30-year mortgage interest rate plan, requiring a methodical and sustained effort. In the same way, addressing mental health should be approached with a long-term perspective, focusing on sustained, gradual improvement rather than quick fixes.
Together, by understanding these hidden struggles and unique analogies, we can better support those around us facing depression and addiction. It’s about making connections, learning, and being there, one fact at a time.
How to fight depression and addiction?
Managing depression and addiction together often means addressing both issues at the same time. Therapy, medication, support groups, and lifestyle changes like exercise and healthy eating can all play vital roles. It’s also important to reach out for help from professionals who have experience with both conditions.
How does living with a depressed person affect you?
Living with a depressed person can be really tough and might strain relationships and family dynamics. You might feel frustrated or at a loss about how to help. Connecting with a support group and talking to others in the same boat can provide some relief and guidance.
What are the symptoms of severe depression?
Severe depression comes with symptoms like struggling to concentrate, remember things, or make decisions. You might have trouble sleeping or end up sleeping too much. Appetite changes, unexplained physical pains, and feelings of worthlessness, hopelessness, or thoughts about death can also be part of severe depression.
How does depression affect daily functioning?
Depression impacts daily life by disrupting sleep patterns, appetite, and energy levels. People can feel worthless, hopeless, and might struggle with concentration and decision-making. These symptoms can make it hard to do everyday tasks like work or even basic self-care.
Are depression and addiction linked?
Depression and addiction often go hand-in-hand because they can amplify each other. Many people might turn to substances to cope with depressive feelings, but substance use can, in turn, worsen depression. About one-third of people with major depression also have trouble with alcohol.
How to snap out of depression?
Just snapping out of depression isn’t something you can do on command. It usually requires a combination of therapy, medication if prescribed, support from loved ones, and lifestyle changes. Patience and time are key components in finding a way out.
What not to tell to a depressed person?
Telling a depressed person to “snap out of it” or “just cheer up” is not helpful and can actually make them feel worse. Instead, offer support, listen without judgment, and encourage them to seek professional help.
Should you let a depressed person sleep all day?
While sleep is important, letting a depressed person sleep all day might actually worsen their symptoms. Encourage a regular sleep schedule that includes a balance. Too much or too little sleep can both exacerbate depression.
What happens if depression is left untreated?
Left untreated, depression can become more severe and lead to significant health issues. It can affect every aspect of a person’s life, including relationships, work, and physical health, making recovery even harder.
What is the last stage of depression?
The last stage of depression can lead to a pervasive sense of hopelessness and the belief that things will never improve. Without intervention, this stage can be extremely dangerous due to the heightened risk of suicidal thoughts.
What is the most harmful depression?
The most harmful form of depression is major depressive disorder. It can completely disrupt a person’s life and significantly increase the risk of suicide if untreated.
What are the 4 levels of depression?
Depression is often classified into four levels: mild, moderate, severe, and major. Each level has increasing symptoms and levels of impairment in daily life, requiring specific treatment approaches.
What makes depression worse?
Depression can worsen due to stress, lack of social support, unhealthy lifestyle choices, and not sticking to a treatment plan. Substance abuse and avoiding medications or therapy can also make symptoms more severe.
What happens to most people with depression?
Many people with depression experience not just emotional but physical symptoms like aches and pains. Without proper treatment, these symptoms can persist and worsen over time, impacting overall health and quality of life.
What often triggers depression?
Depression can be triggered by various factors, including genetic predisposition, traumatic events, chronic stress, and significant life changes. It’s a complex condition with multiple potential causes.
What are 3 ways to overcome addiction?
Overcoming addiction might involve seeking professional help, establishing a strong support network, and engaging in behavioral therapies. Combining these approaches increases the chances of successful recovery.
What are three strategies for coping with depression?
Three strategies for coping with depression include therapy, lifestyle changes like regular exercise and healthy eating, and building a strong support system of friends or support groups to lean on.
How do I get rid of extreme addiction?
Extreme addiction requires comprehensive treatment, including detoxification, therapy, support groups, and sometimes medication-assisted treatment. Professional help is crucial in developing a sustainable recovery plan.
How to get out of depression naturally?
Natural ways to combat depression include regular physical activity, maintaining a balanced diet, practicing mindfulness or meditation, and ensuring adequate sleep. Building a routine and staying connected socially can also help.