When approaching the sensitive and crucial work of supporting parents of children struggling with addiction, trauma-informed care becomes an essential framework. Recognizing the pervasive impact of trauma, this approach involves integrating an understanding of trauma into policies, procedures, and practices. Here, we delve into the five guiding principles of trauma-informed care and how they can transform the way we support and advocate for families affected by addiction.
1. Safety: Creating a Secure Environment for Healing
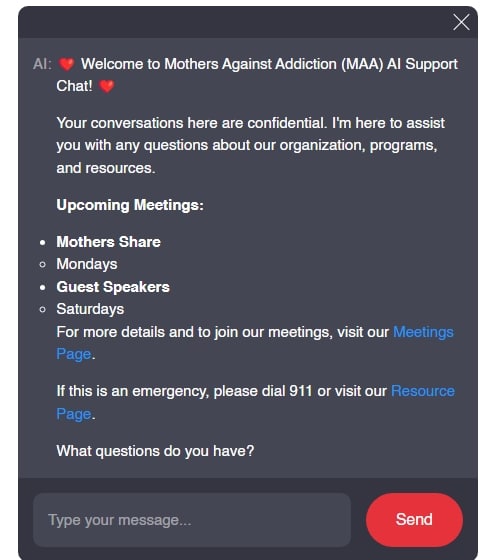
Safety is the cornerstone of trauma-informed care. For parents and children grappling with addiction-related trauma, creating a physical and emotional safe space is paramount. Organizations like Mothers Against Addiction strive to provide environments where parents feel protected from emotional harm, judgment, and stigma. By offering secure spaces, whether through support groups, therapy sessions, or online forums, we allow families to begin their healing journey without fear. Physical spaces, such as those designed by the Center for Youth Wellness, use soothing colors and private seating areas to offer a sense of comfort and security, exemplifying how critical a safe atmosphere is.
Safety isn’t just about physical spaces; it’s also about creating emotional, social, and psychological safety. Providing avenues where parents feel heard, validated, and free from judgment enables a more genuine healing process. Through continuous dialogue and active listening, trauma-informed care ensures that no parent or child feels isolated or misunderstood. Creating a secure environment for healing is the first step towards breaking the cycle and fostering resilience.
2. Trustworthiness and Transparency: Building Credible Relationships
Trustworthiness and transparency underpin the interactions between caregivers, support organizations, and families. Building trust means being open about intentions, practices, and policies. For example, the Betty Ford Center openly shares its treatment methodologies and outcomes with families, fostering reliability and confidence. Transparency in communication and actions reduces the feelings of uncertainty and suspicion that often accompany trauma, making it easier for families to engage in the recovery process.
Establishing trust requires time and consistent effort. When organizations provide clear, understandable information on treatment options, potential risks, and expected outcomes, families feel more secure in their choices. The goal is to create an environment where parents know they are receiving accurate and comprehensive information, essential for informed decision-making. By fostering a culture of honesty and openness, trauma-informed care helps build sturdy bridges between caregivers and those they serve.
In any relationship, transparency is the linchpin that holds trust in place. Without it, even well-meaning interventions can fall flat. Through trustworthiness and transparency, families gain the confidence to invest wholeheartedly in the recovery journey.
| Aspect | Description |
|---|---|
| Definition | Trauma-informed care is a framework for human service delivery based on understanding how trauma affects people’s lives and service needs. |
| Five Guiding Principles | 1. Safety (physical and emotional) 2. Trustworthiness and Transparency 3. Choice 4. Collaboration and Mutuality 5. Empowerment and Voice |
| Five R’s of Trauma-Informed Care | 1. Realize: Recognize the widespread impact of trauma 2. Recognize: Identify signs and symptoms of trauma 3. Respond: Integrate trauma knowledge into practices 4. Resist Re-traumatization: Actively work to prevent re-traumatization |
| Key Focus | Shift the perspective from asking “What’s wrong with you?” to “What has happened to you?” |
| Application Settings | Can be applied in clinical/mental health care settings, workplaces, educational institutions, and other organizations. |
| Core Intentions | 1. Realize: Widespread impact of trauma and paths for recovery 2. Recognize: Signs/symptoms in patients, families, and staff 3. Respond: Integrate trauma understanding into policies, procedures, and practices 4. Resist Re-traumatization: Prevent further harm actively |
| Foundational Authors | Drs. Maxine Harris and Roger Fallot |
| Implementation | Organizations need to fully integrate awareness of individual, historical, racial, and systemic trauma into all aspects of functioning. |
| Expected Outcomes | Reducing the likelihood of re-traumatization, fostering a healing environment, and improving service delivery and patient outcomes. |
3. Peer Support: The Power of Shared Experiences
Peer support is an invaluable resource within trauma-informed care, offering individuals the opportunity to connect with others who have faced similar challenges. Groups like Narcotics Anonymous or community-based organizations such as Mothers Against foster peer support networks, where parents can share experiences, advice, and encouragement. This collective experience aids in reducing isolation and provides authentic, empathetic support that is often more relatable and impactful than professional guidance alone.
The power of shared experiences cannot be overstated. When parents interact with others who have faced similar struggles, it validates their feelings and offers hope. Testimonies from those who have navigated the turbulent waters of addiction can be incredibly inspiring and reassuring. Through peer support, families realize they are not alone in their fight—there’s a community ready to uplift and guide them.
Building a robust network of peer support involves training and empowering peer advocates who can share their insights and experiences in meaningful ways. Peer support transforms the journey of recovery from a solitary path into a shared voyage of healing and growth.
4. Collaboration and Mutuality: Engaging Families as Partners
Trauma-informed care emphasizes collaboration and mutuality, shifting the dynamic from a ‘helper-and-helped’ model to one of partnership. Families should be seen as partners in the process, with their insights and experiences valued equally. Organizations like the Substance Abuse and Mental Health Services Administration (SAMHSA) promote programs that emphasize family involvement in treatment planning and decision-making, reflecting a mutual approach where caregivers and clients work together toward recovery.
Collaboration means more than just involving families in decisions—it’s about truly valuing their input and making them co-creators of their recovery plans. This participatory approach empowers families and helps tailor interventions to better suit individual needs. Engaging families as partners fosters a sense of shared responsibility and commitment, crucial for sustained recovery.
In trauma-informed settings, mutuality creates a synergistic relationship where everyone’s voice is heard, and all contributions are respected. This collaborative model not only enhances the effectiveness of care but also strengthens the family unit, building a foundation of trust and solidarity.
5. Empowerment, Voice, and Choice: Uplifting and Advocating for Families
Empowerment, voice, and choice are critical components of trauma-informed care, focusing on enhancing the individual’s strengths and resilience. Empowering parents and children means providing them with the tools, resources, and opportunities to make informed choices about their care and recovery. Advocacy work, such as that carried out by Facing Addiction with NCADD, emphasizes giving families a platform to voice their needs and preferences, thereby tailoring support to better meet those needs and fostering a sense of control and autonomy in their recovery journey.
Empowerment involves recognizing and nurturing the inherent strengths within families, helping them rebuild their lives with dignity and hope. Providing choice allows families to explore various pathways to recovery, ensuring they find the most suitable approach for their unique circumstances. This principle is rooted in the belief that every individual has the capacity for change and growth when given the right support.
Voice and choice go hand-in-hand, creating an environment where families feel respected and valued. By focusing on empowerment, trauma-informed care not only aids healing but also instills a sense of independence, resilience, and self-efficacy in all involved.
The Future of Trauma-Informed Care
The principles of trauma-informed care are not static; they evolve with ongoing research and practical application. As our understanding of trauma deepens, so too must our commitment to integrating this knowledge in every facet of support and advocacy work. At Mothers Against Addiction, we are dedicated to continuously learning and adapting to best serve the families we support.
By embracing these five guiding principles, we can create a more compassionate, effective, and responsive system of care. This approach aids healing and empowers families to rebuild their lives with dignity and hope. Let us move forward with a heightened awareness of the profound impact of trauma-informed care, ensuring that every family affected by addiction receives the understanding, respect, and support they deserve.
As we reflect on the transformative potential of trauma-informed care, we envision a future where every interaction, policy, and practice is infused with an understanding of trauma’s impact. By steadfastly adhering to the principles of safety, trustworthiness, peer support, collaboration, and empowerment, we can chart a path toward resilience and recovery for families and communities nationwide. Together, we can create environments that not only care for but genuinely understand and advocate for those affected by addiction.
Trauma-informed Care Five Guiding Principles
Fascinating Tidbits and Trivia
Let’s dive into some intriguing facts that can give us a broader understanding of trauma-informed care. Did you know that self-esteem issues often play a huge role in addiction? Trauma-informed care tries to address not just the addiction itself but also the underlying psychological scars, such as those related to self-esteem And addiction.( By boosting a child’s self-worth, we can help mitigate the risk of relapse and promote long-term recovery.
Now, speaking of overcoming adversity, trauma can stem from myriad sources. Even celebrities aren’t immune. Take Harry And Meghan,( for example. They’ve faced immense public scrutiny, which has impacted their mental health. Trauma-informed care acknowledges that trauma can come from anywhere—from childhood abuse to intense public scrutiny—and tailors its approach to factor in these unique stressors.
Transitioning from celebrities to sports icons, can you believe that NFL Hall of Famer Orlando Pace( once suffered from significant personal trauma following his retirement? Athletes, despite their legendary status, are not invincible to the psychological strain that can lead to addiction. Trauma-informed care provides the kind of holistic, compassionate approach required to support individuals through their mental health struggles.
Additionally, PTSD is another significant factor linked to both trauma and addiction. Trauma-informed care targets these interdependencies by understanding the deep-seated roots of these issues. Consider how vital this approach is when addressing Ptsd And addiction.( By focusing on the trauma that often underpins these conditions, care providers can develop more effective treatment plans that go beyond merely addressing the symptoms.
In a lighter vein, did you know that even sports statistics can reflect moments of stress and trauma? Just look at Man united Vs Aston villa Stats.( For some fans, these games are more than just numbers; they can elicit memories of triumph or heartbreak that have a lasting impact. The emotional rollercoaster of sports fandom illustrates how deeply emotional experiences can shape our lives, another key tenet of trauma-informed care. Even seemingly minor events can leave long-lasting scars that necessitate a thoughtful, empathetic approach to healing.
These stories and facts underline how trauma-informed care casts a wide net in addressing the complex tapestry of human experiences. It’s not just about treating the symptoms but understanding the people behind those symptoms—their traumas, their stories, their battles, and their victories.
What are the 5 principles of trauma-informed care?
The five principles of trauma-informed care are safety, choice, collaboration, trustworthiness, and empowerment. These principles aim to create a supportive environment by addressing both physical and emotional safety, providing options, fostering collaboration, being trustworthy, and empowering individuals.
What is meant by trauma-informed care?
Trauma-informed care means understanding how trauma affects people’s lives and their needs. It’s about creating services that consider their trauma histories, focusing on providing a sense of safety and not re-traumatizing them.
What are the 4 elements of trauma-informed care approach?
The four elements of a trauma-informed care approach are realizing the widespread impact of trauma, recognizing the signs and symptoms of trauma, responding by integrating knowledge about trauma into practices, and resisting re-traumatization.
What is an example of trauma-informed care?
One example of trauma-informed care is a medical clinic ensuring their staff receives training on recognizing trauma signs and symptoms. They create a welcoming and safe environment, offer choices in treatment, and maintain consistent and transparent communication.
What are the 4 C’s of trauma-informed care?
The four C’s of trauma-informed care are connection, compassion, collaboration, and competence. These elements guide the approach in building trusting relationships, showing empathy, working together with individuals, and being skilled in trauma-informed practices.
What are the 6 C’s trauma?
The six C’s of trauma-informed care include safety, trustworthiness, peer support, collaboration and mutuality, empowerment and choice, and cultural, historical, and gender issues. These principles provide a comprehensive framework to support individuals with trauma histories.
What best describes trauma-informed care?
Trauma-informed care best describes an approach that recognizes and responds to the effects of all types of trauma. It emphasizes physical and emotional safety and creates opportunities for survivors to rebuild a sense of control and empowerment.
What trauma-informed care is not?
Trauma-informed care is not about treating trauma itself but creating an environment that recognizes trauma’s impact and seeks to avoid re-traumatizing individuals. It focuses on understanding and responding to trauma, not diagnosing or therapy.
How to practice trauma-informed care?
To practice trauma-informed care, one should educate themselves about trauma, create a safe and welcoming environment, support empowerment and choice, communicate transparently, and collaborate with individuals affected by trauma.
What are the 5 S’s of trauma-informed care?
The five S’s of trauma-informed care aren’t commonly referenced, but the five principles include safety, choice, collaboration, trustworthiness, and empowerment, which are critical guidelines for providing supportive care to trauma survivors.
What are the 4 P’s of trauma?
The four P’s of trauma are preparedness, planning, prevention, and protection. These elements help organizations and individuals anticipate and respond to trauma impacts effectively.
What behaviors align with trauma-informed care?
Behaviors that align with trauma-informed care include showing empathy and genuine care, being transparent, offering choices, actively listening, collaborating with the person, and consistently working to build trust and safety.
How do you explain trauma-informed?
Trauma-informed means understanding trauma, its effects on people, and incorporating that awareness into how we interact and provide services. It’s shifting our question from “What’s wrong with you?” to “What happened to you?”
What is the difference between trauma and trauma-informed care?
The difference between trauma and trauma-informed care is that trauma refers to the actual experiences that cause distress and harm, while trauma-informed care is an approach that aims to support and address the needs resulting from those experiences without causing further harm.
What are examples of trauma-informed questions?
Examples of trauma-informed questions include “Can you share what happened that led you here?” “What can we do to support you best?” and “Are there things that make you feel unsafe or uncomfortable?”
What are the 5 S’s of trauma-informed care?
The five principles of trauma-informed care are safety, choice, collaboration, trustworthiness, and empowerment. These principles aim to create a supportive environment that addresses both physical and emotional safety and promotes healing.
What are the 5 trauma-informed practices?
The five trauma-informed practices include recognizing the impact of trauma, creating a safe environment, supporting choice and control, collaborating meaningfully, and empowering individuals to take an active role in their care and recovery.
What are the 5 areas of trauma?
The five areas of trauma often referred to include physical trauma, emotional trauma, psychological trauma, historical trauma, and complex trauma. These areas cover a range of trauma experiences people might endure.
What are the six pillars of trauma-informed care?
The six pillars of trauma-informed care include safety, trustworthiness and transparency, peer support, collaboration and mutuality, empowerment and choice, and cultural, historical, and gender issues. These pillars provide a solid foundation for creating supportive and effective care environments.