When it comes to access to treatment, the landscape can feel daunting. In 2024, the conversation isn’t just about addiction as a health issue; it’s about ensuring that everyone, regardless of background or circumstances, can receive the care they need. Too many families, like those behind Mothers Against addiction, strive for justice in addiction treatment access while wrestling with their own grief and pain. The facts are stark: people from marginalized communities encounter significant hurdles in obtaining effective treatment for substance use disorders.
As more parents face the heart-wrenching challenge of watching their children struggle with addiction, it’s clear we need to turn awareness into action. Families shouldn’t have to battle not just the addiction itself but also a fragmented and inequitable treatment system. Those in need deserve quality care that respects their dignity and offers the promise of recovery. Together, we can push for reforms that bridge the gaps in access to treatment.
The Landscape of Access to Treatment in 2024
Access to treatment is multifaceted, shaped by a range of sociopolitical factors. The conversation has evolved beyond just biological factors of addiction; it’s now clear that social standing, location, and even structural healthcare disparities play crucial roles in access. Research indicates that those from lower-income backgrounds or rural areas face severe barriers, making it much harder for them to find the help they desperately need.
Take the example of rural Ohio, which, according to the National Institute on Drug Abuse, sees fewer treatment centers compared to its urban counterparts. People needing support may go hours without finding a facility equipped to help them. This situation leaves many feeling isolated in their struggle. Families with children facing addiction issues often find themselves at a crossroads, with limited options and even more limited hope.
Access to treatment is further complicated by insurance disparities. While the Affordable Care Act enabled many to get insurance coverage, a significant number remain uninsured or underinsured. States that chose not to expand Medicaid have shown higher rates of untreated addiction, a clear signal that access to treatment remains uneven. The policies designed to rectify this inequity haven’t fully reached all communities, and it’s time for that to change.
Top 7 Factors Influencing Access to Treatment for Addiction
Understanding the landscape of access to treatment reveals several key barriers. Here are seven factors that significantly influence the level of support available for those fighting addiction:
Access to treatment is not just about the facilities; it’s about creating networks and resources that can reach underserved populations effectively. Understanding these barriers is the first step toward creating a more equitable system that supports all individuals facing addiction.
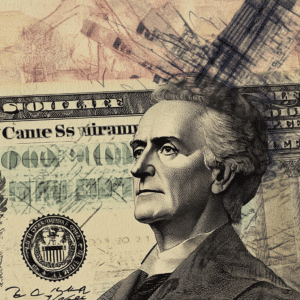
| **Category** | **Description** |
|---|---|
| Access to Treatment Initiative | A collaborative program allowing treatment costs to be shared among the patient, pharmaceutical companies, and other parties based on the patient’s ability to pay. |
| Access to Medicines | Ensures that all individuals can reasonably obtain needed medications to maintain health, recognized as part of the right to health since 1946. |
| Health Care Access | Involves the ability to obtain necessary healthcare services (prevention, diagnosis, treatment) that are affordable, convenient, and timely. |
| Key Components | – Insurance Coverage: Essential for reducing out-of-pocket costs and improving access to services. – Timeliness of Care: Access to care should be quick to prevent worsening health conditions. – Accessibility of Primary and Preventive Care: Availability of local services to manage health proactively. |
| Impact of Lack of Insurance | Leads to poorer health outcomes, especially for chronic diseases requiring ongoing treatment, creating a financial burden on families. |
| Statistics (U.S.) | – Approximately 33 million Americans are uninsured as of 2023. – Individuals without insurance are more likely to postpone seeking medical care. |
| Financial Strain from Treatment | Patients with chronic conditions may face costs exceeding $1,000/month for medications and treatments, often leading to tough financial decisions. |
| International Right to Health | Recognizes the obligation of states to ensure access to essential medicines and healthcare services as fundamental for improving population health. |
Innovations and Strategies to Enhance Access to Treatment
As we witness ongoing challenges, several innovative strategies are emerging to improve access to treatment. These initiatives focus on leveraging technology, community engagement, and policy reform to address existing gaps:
Fostering these innovative models can help dismantle barriers and create a more integrated system of care. It’s high time we break the cycles of inequity in access to treatment, ensuring that every individual has a fighting chance against addiction.
The Road Ahead: Rethinking Access to Treatment Amidst Ongoing Challenges
Navigating access to treatment in 2024 requires a consistent focus on justice and equity. It’s about more than just ensuring everyone gets help; it’s about making sure that help is effective and compassionate. Advocating for systemic changes involves coming together as a community, sharing stories, and standing strong in the fight for inclusion and equal rights within treatment access.
As parents within the Mothers Against Addiction community know all too well, we must never underestimate the power of collective advocacy. Access to treatment needs to shift toward a more inclusive, respectful approach that acknowledges the social determinants of health. With ongoing community involvement, dedication to innovative care models, and a relentless push for legislative change, we can reduce the barriers faced by those in dire need.
In closing, the quest for equitable access shouldn’t be a lonely road. Together, we can forge paths that lead to comprehensive care, helping families reclaim their lives from the clutches of addiction. Finding ways to stretch our resources and advocate for change enriches not only the lives of those struggling but also uplifts our whole society, creating a more compassionate and understanding environment for all.
As you navigate this landscape, remember, you’re not alone. Our community at Mothers Against addiction is here to support you every step of the way. Together, we can change the narrative around access to treatment, making sure that no family has to fight this battle in isolation.
Access to Treatment: Fun Facts and Insights
The Journey Towards Better Access to Treatment
Access to treatment for addiction has grown into a key focus for improving health equity. Did you know that mental health parity laws play a big role in this? These laws mandate that health insurance plans cover mental health services, including addiction treatment, on par with physical health services. This means that more people have a shot at getting the help they need without facing extra financial hurdles. Just think about it: with mental health issues affecting millions, these laws can make a real difference.
Now, shifting gears a bit—ever heard of safe injection Sites? These facilities aim to reduce the risks associated with drug use, providing a safe environment where individuals can use substances under supervision. This can significantly decrease the likelihood of overdose and transmission of diseases. Just like when you tune into a football game, hoping the score shifts in your favor, access to treatment is about creating those winning conditions for individuals facing addiction.
Breaking Down Barriers in Treatment Access
When discussing access to treatment, it’s essential to consider how the decriminalization Of Drugs can remove stigma and encourage those struggling with addiction to seek help. By treating addiction more like a health care issue rather than a criminal one, communities can foster environments that support recovery and healing. Imagine if more people saw accessing treatment as a normal part of life, just like figuring out gross income Vs net income—it’s all about knowing the details to make informed decisions!
You might think access to treatment is a far-off concept, but many local initiatives aim to level the playing field. Just like the character Calcifer in “Howl’s Moving Castle, who lights up the room with his fiery spirit, these efforts strive to light up pathways for those needing help. Remember, every little bit counts. With enough community support and effective policies, we can break down the barriers that have kept too many people from accessing the treatment they deserve.
What is the meaning of access to medicine?
Access to medicine means having the ability to get the medicines you need to stay healthy. It’s recognized as a part of the right to health, which has been supported by international law since 1946.
What is the meaning of access to care?
Access to care refers to being able to get necessary healthcare services like check-ups, treatments, and ongoing management for health issues. It’s important that these services are both affordable and easy to reach for everyone.
What are the three components of access to care?
The three main components of access to care are having insurance coverage, receiving timely care, and ensuring that primary and preventive healthcare services are easy to access. These elements help ensure people can get the care they need when they need it.
Why is lack of access to healthcare a problem?
Lack of access to healthcare is a problem because it can lead to poor health outcomes. When people can’t get the treatment or management they need for chronic conditions, it can create financial strains and worsen their overall health.
What is access in medical terms?
In medical terms, access refers to how easily people can obtain healthcare services. This includes factors like availability of providers, affordability of treatments, and the ability to get to healthcare facilities.
What is an example of access to healthcare?
An example of access to healthcare is having a local clinic where individuals can get routine check-ups and vaccinations without facing long travel times or high costs.
Is access to medical care a right?
Access to medical care is considered a right by many advocates, as everyone should be able to get the healthcare services they need to maintain their health and well-being.
What is the meaning of patient access?
Patient access means how well a patient can obtain healthcare services. This includes being able to see doctors, get prescriptions filled, and receive necessary treatments without significant barriers.
What are the 5 dimensions of access to healthcare?
The five dimensions of access to healthcare include availability, accessibility, accommodation, affordability, and acceptability. Each one plays a critical role in determining how easily someone can get healthcare.
Which is a measure of access to care?
A measure of access to care could be the percentage of people who have health insurance, as this often influences their ability to access necessary services.
What can limit access to healthcare services?
Several factors can limit access to healthcare services, including lack of health insurance, high costs of treatment, limited availability of providers, or long travel distances to healthcare facilities.
What is the definition of accessible care?
Accessible care means healthcare services that are easy for everyone to reach and use, considering aspects like location, cost, and availability. It should be designed to meet the needs of all community members.
How to fix access to healthcare?
To fix access to healthcare, we can increase insurance coverage, improve healthcare infrastructure, reduce costs, and ensure there’s a sufficient number of healthcare providers to meet community needs.
What does access to care mean?
Access to care means having the ability to obtain necessary healthcare services in a timely, affordable, and convenient manner. It’s about breaking down barriers to ensure everyone can get the help they need.
What is the biggest barrier to healthcare access?
The biggest barrier to healthcare access is often the cost, which includes high insurance premiums, out-of-pocket expenses for treatments, and the price of medications, making it difficult for many folks to get necessary care.
What is access medicine used for?
Access medicine is used for initiatives that aim to improve access to essential medicines, helping share the costs among patients, pharmaceutical companies, and other parties based on what the patient can afford.
What is the definition of drug access?
The definition of drug access refers to the ability of patients to obtain the medications they need for their health conditions. This involves affordability and availability in their region.
Why is access to medication important?
Access to medication is important because it ensures that individuals can follow through on their treatment plans, manage chronic conditions, and maintain their overall health and well-being.
What is early access to medicines?
Early access to medicines means making new treatments available to patients before they are widely released to the public, often used in cases of serious health conditions where time is of the essence.