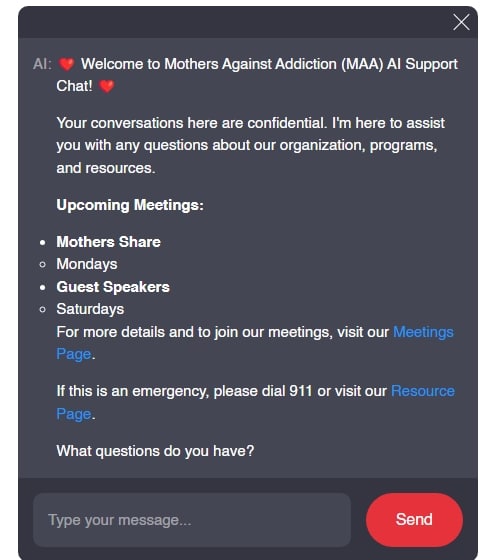
Navigating insurance coverage for rehab can feel like wandering through a maze. Myths and misconceptions often cloud the path to understanding what treatment really entails and who pays for it. For parents grappling with a child struggling with addiction, this uncertainty can be intimidating. As we dive deeper into the myths surrounding rehab coverage, we’ll offer clarity – because every step towards understanding brings hope for better outcomes.
1. Top 5 Myths About Insurance Coverage for Rehab You Should Know
Misunderstandings about insurance coverage for rehab can create barriers for individuals and families seeking help. Let’s unpack some common myths:
Myth 1: All Rehab Centers Are Covered by Insurance
One common misconception is that all treatment facilities are covered by every insurance plan. Surprise! Not every rehab center falls under your policy’s network. For example, while luxury facilities like Promises Malibu might offer exceptional care, they may only have limited coverage options. In contrast, organizations like the Hazelden Betty Ford Foundation usually take a wide range of insurance, making them more accessible for families navigating tough times.
Myth 2: Insurance Covers All Types of Treatment
People often think that every kind of therapy or service is covered by insurance – think again! While traditional evidence-based treatments usually get the nod, alternative therapies can sometimes be overlooked. For instance, Equine Therapy might be beneficial for some, but depending on your insurance company, it could be left off the treatment list when it comes to coverage.
Myth 3: You Must Be Substance-Free to Get Help
It might shock some to hear that many believe a person has to be sober to qualify for treatment. In reality, that’s far from the case! Treatments like medically supervised detox are specifically designed for those currently using substances, including alcohol and opioids. They’re an essential part of the recovery process and are typically covered under most plans, ensuring safety while starting the healing journey.
Myth 4: Insurance Coverage for Rehab Is Always Quick
The hope of immediate approval for rehab once inside a facility is a comforting thought, but the reality is a bit more complex. Many insurance providers, like UnitedHealthcare and Cigna, require evaluations for medical necessity, which can elongate the approval process. Families are often met with waiting periods that can feel frustrating – but understanding this process is helpful for setting expectations.
Myth 5: Only Inpatient Programs Are Covered
Many families assume that if they want coverage, they have to choose inpatient options, but that’s not true! Many insurance policies provide coverage for outpatient programs, especially when the addiction is less severe. Carriers like Aetna and Blue Cross Blue Shield (BCBS) both offer various outpatient services, recognizing that not everyone needs a residential stay to recover.
2. What Is Medical Necessity and Its Role in Insurance Coverage for Rehab?
Understanding the concept of medical necessity is crucial for navigating insurance coverage for rehab. Insurers define this as services that a qualified healthcare professional considers essential for diagnosis or treatment. Here’s what that means in practical terms:
| **Topic** | **Details** |
|---|---|
| Insurance Coverage for Rehab | |
| Common Denial Reasons | 1. Treatment deemed as lacking medical necessity 2. Utilization of out-of-network providers 3. Incomplete or insufficient documentation |
| Tax Deductions | – Medical expenses, including rehab for drug addiction or alcoholism, may be deductible from taxable income according to IRS guidelines. |
| Coverage Types | 1. Inpatient treatment 2. Outpatient treatment 3. Detoxification services |
| Insurance Providers | – Major private insurers (e.g., Aetna, UnitedHealthcare, Blue Cross Blue Shield) – Medicaid and Medicare (conditions may vary) |
| Coverage Limitations | – Varies by plan; may include a limit on the number of treatment days, specific providers, or types of therapies covered. |
| Financial Assistance | – Some rehab facilities offer sliding scale fees, scholarships, or payment plans for those without insurance. – Nonprofits and local resources can provide financial aid. |
| Life Insurance for Recovering Addicts | – Recovering addicts can purchase term life insurance, but may face challenges in securing coverage and incur higher premiums. |
| Premium Adjustments | – Premiums may be higher based on risk assessment performed by insurers, considering the individual’s recovery history and time sober. |
| Pre-existing Conditions | – Insurers may regard addiction as a pre-existing condition, potentially impacting coverage and pricing terms. |
3. Navigating the Insurance Landscape for Rehab Coverage
Understanding the specifics of your insurance provider is key for making the most of your benefits. Each insurance company has its unique stipulations regarding insurance coverage for rehab services:
Provider Networks
Most insurance plans require you to utilize in-network facilities for maximum benefits. If you use an out-of-network provider, you may face higher out-of-pocket costs. If you’re enrolled with a provider like Anthem, seeking treatment from a partnership facility will yield better financial benefits than going rogue with an out-of-network center.
Coverage Limits and Durations
Insurance coverage for rehab can vary widely between plans when it comes to how long they’ll pay for treatment. For example, Kaiser Permanente may cap coverage at a standard 30-day stay, while others might adapt based on your situation and medical necessity – thus providing you with flexible options during recovery.
Preauthorization Requirements
Before treatment kicks off, many insurance plans require preauthorization. This involves the treatment provider collaborating with the insurance company to justify the need for rehab. Some plans, such as Humana, have stringent guidelines that might influence your access to immediate care.
4. The Benefits of Understanding Your Policy
Taking the time to familiarize yourself with your insurance policy can significantly smooth the recovery journey. Here’s how:
Navigating the Path Forward
Understanding insurance coverage for rehab is not just about breaking down myths; it’s about action. By clarifying the intricate details of insurance plans and grasping the essential notion of medical necessity, families can pursue the full spectrum of care needed for recovery. Staying updated about shifts in policies and the growing acknowledgment of addiction treatment as a medical necessity in 2024 and beyond is crucial for those in need.
Recovery isn’t just a possibility; it’s a journey worth embarking on with hope and support. Let’s ensure that every parent, every child grappling with addiction, finds the clarity they need to pursue healing and strength for the future. For more resources on advocating for addiction recovery, exploring Policies on substance use in pregnancy, and understanding Naloxone accessibility, visit Mothers Against Addiction.
We stand in solidarity, ready to help navigate this path. You are not alone; together, we advocate for those who deserve a second chance, a brighter tomorrow, and the defining strength of resilience.
Insurance Coverage for Rehab: Myths and Medical Necessity
Untangling the Myths of Insurance Coverage for Rehab
One of the most common misconceptions about addiction treatment is that insurance coverage for rehab is a straightforward process. Did you know that around 90% of Americans have some form of health insurance? However, the specifics of coverage can vary widely, leaving many families to feel like they’re in a gripping episode of the One Punch man anime—racing against the clock while battling obstacles. For instance, understanding the difference between Secured Vs unsecured loans can play a crucial role in financing treatment options when insurance doesn’t cover certain services. Meanwhile, insurance can provide a safety net, but it’s essential to check what your policy specifically includes regarding rehab services.
Did you know that nearly two-thirds of those who are fully insured still pay out-of-pocket costs toward addiction treatment? Recognizing this reality can help families prepare for potential expenses while they advocate for addiction recovery. In some state-run programs, such as those often found in Saitama OK, rehab services may even prioritize individuals with minimal financial resources, making it accessible for those who need it most. Understanding these nuances can be key, especially as different rehab facilities work with various insurance providers to deliver treatments.
Facts That Will Surprise You About Rehab Coverage
Interestingly, mental health treatment coverage is often mandated by law—something many people don’t know. This is a silver lining for many facing addiction issues. The reality is, not every plan will be the same; some might cover detox, while others may not. A study found that facilities associated with certain wellness services, like Silverleaf Resorts, are more likely to have comprehensive coverage options. Isn’t it comforting to think that while our loved ones battle addiction, assistance is available through insurance to help cushion the fall?
Additionally, did you know that some rehab centers, particularly luxury ones, may not accept insurance at all? So, families might need to explore alternative financing options like loans or payment plans for treatment. This brings to light the importance of knowing the true costs ahead of time. After all, it’s critical for families to gather information and navigate through the maze while staying informed about what their insurance will actually provide. Whether you’re discovering famous Virgos or the growing relationship between entertainment and wellness, knowledge is power when ensuring access to necessary care.
Why do insurance companies deny rehab?
Insurance companies often deny rehab if they think the treatment isn’t medically necessary, if it’s being done with out-of-network providers, or if there’s incomplete documentation from the healthcare provider.

Is rehab a deductible medical expense?
You can deduct medical expenses from your taxable income, and rehab for drug addiction or alcoholism fits the bill as a medical expense according to the IRS.

Does rehab affect life insurance?
Recovering addicts can get term life insurance, but they might run into some bumps along the way, like higher premiums or extra requirements due to their history.
How much does it cost a person on average for inpatient rehabilitation in the state of Wisconsin?
In Wisconsin, the average cost for inpatient rehabilitation can be around $15,000 to $30,000 for a 30-day program, but this can vary depending on the facility and services offered.
What is insurance company rehabilitation?
Insurance company rehabilitation generally refers to programs that help policyholders recover from injuries or illnesses while allowing claims for certain treatments and therapies.
What does rehabilitation mean in insurance?
In the insurance world, rehabilitation means getting a person back to their pre-accident or pre-illness condition, often focusing on physical or occupational therapy to aid recovery.
What are the rehabilitation expenses?
Rehabilitation expenses can cover various costs like therapy sessions, medications, and sometimes even transport to treatment centers, but this depends on individual policies and circumstances.
What Cannot be claimed as a medical expense?
You can’t claim expenses like cosmetic procedures, healthy foods, or gym memberships as medical expenses since they’re not primarily for treating a medical condition.
What are not qualified medical expenses?
Not qualified medical expenses include things like over-the-counter medications without a doctor’s prescription, or expenses considered cosmetic or non-essential, like teeth whitening.
Is it ever too late for rehab?
It’s never too late for rehab; many folks find help and strength to change their lives regardless of their age or how long they’ve been struggling.
Can I get life insurance if I take suboxone?
If you take suboxone, you can still get life insurance, but expect some challenges and possibly pay more, as insurance companies might consider your medication as a risk factor.
Does alcoholism void life insurance?
Alcoholism doesn’t automatically void life insurance, but it may lead to higher premiums or certain exclusions based on your history.
How many days does Medicare allow for rehab?
Medicare usually covers up to 100 days of rehab in a skilled nursing facility, but that depends on meeting certain criteria.
How much does rehabilitation cost in USA?
Rehabilitation costs in the USA generally range widely, with prices averaging from $20,000 to $50,000 for a month, but can vary widely based on location, type of facility, and specifics of the program.
How much is alcohol rehab in Wisconsin?
In Wisconsin, alcohol rehab can cost about $1,500 to $12,000 for a typical 30-day stay, depending on the level of care and facility type.
Why would insurance deny physical therapy?
Insurance might deny physical therapy if they think the treatment doesn’t relate to an injury covered by the policy or if they find the documentation lacking.
Why do health insurance companies deny their patients?
Health insurance companies may deny patients if they believe the treatment isn’t necessary, the patient isn’t eligible, or if there are issues with documentation and compliance.
Why would Medicare deny rehab?
Medicare might deny rehab if the service isn’t deemed medically necessary, if you’ve reached the limit of covered days, or if you don’t meet specific criteria for inpatient care.
Why do insurance companies deny medications?
Insurance companies might deny medications for reasons like lack of prior authorization, if the drug isn’t covered under the plan, or if it hasn’t been proven effective for the patient’s specific condition.

Why do insurance companies deny rehab?
Insurance companies often deny rehab if they think the treatment isn’t medically necessary, if it’s being done with out-of-network providers, or if there’s incomplete documentation from the healthcare provider.
Is rehab a deductible medical expense?
You can deduct medical expenses from your taxable income, and rehab for drug addiction or alcoholism fits the bill as a medical expense according to the IRS.
Does rehab affect life insurance?
Recovering addicts can get term life insurance, but they might run into some bumps along the way, like higher premiums or extra requirements due to their history.
How much does it cost a person on average for inpatient rehabilitation in the state of Wisconsin?
In Wisconsin, the average cost for inpatient rehabilitation can be around $15,000 to $30,000 for a 30-day program, but this can vary depending on the facility and services offered.
What is insurance company rehabilitation?
Insurance company rehabilitation generally refers to programs that help policyholders recover from injuries or illnesses while allowing claims for certain treatments and therapies.
What does rehabilitation mean in insurance?
In the insurance world, rehabilitation means getting a person back to their pre-accident or pre-illness condition, often focusing on physical or occupational therapy to aid recovery.
What are the rehabilitation expenses?
Rehabilitation expenses can cover various costs like therapy sessions, medications, and sometimes even transport to treatment centers, but this depends on individual policies and circumstances.
What Cannot be claimed as a medical expense?
You can’t claim expenses like cosmetic procedures, healthy foods, or gym memberships as medical expenses since they’re not primarily for treating a medical condition.
What are not qualified medical expenses?
Not qualified medical expenses include things like over-the-counter medications without a doctor’s prescription, or expenses considered cosmetic or non-essential, like teeth whitening.
Is it ever too late for rehab?
It’s never too late for rehab; many folks find help and strength to change their lives regardless of their age or how long they’ve been struggling.
Can I get life insurance if I take suboxone?
If you take suboxone, you can still get life insurance, but expect some challenges and possibly pay more, as insurance companies might consider your medication as a risk factor.
Does alcoholism void life insurance?
Alcoholism doesn’t automatically void life insurance, but it may lead to higher premiums or certain exclusions based on your history.
How many days does Medicare allow for rehab?
Medicare usually covers up to 100 days of rehab in a skilled nursing facility, but that depends on meeting certain criteria.
How much does rehabilitation cost in USA?
Rehabilitation costs in the USA generally range widely, with prices averaging from $20,000 to $50,000 for a month, but can vary widely based on location, type of facility, and specifics of the program.
How much is alcohol rehab in Wisconsin?
In Wisconsin, alcohol rehab can cost about $1,500 to $12,000 for a typical 30-day stay, depending on the level of care and facility type.
Why would insurance deny physical therapy?
Insurance might deny physical therapy if they think the treatment doesn’t relate to an injury covered by the policy or if they find the documentation lacking.
Why do health insurance companies deny their patients?
Health insurance companies may deny patients if they believe the treatment isn’t necessary, the patient isn’t eligible, or if there are issues with documentation and compliance.
Why would Medicare deny rehab?
Medicare might deny rehab if the service isn’t deemed medically necessary, if you’ve reached the limit of covered days, or if you don’t meet specific criteria for inpatient care.
Why do insurance companies deny medications?
Insurance companies might deny medications for reasons like lack of prior authorization, if the drug isn’t covered under the plan, or if it hasn’t been proven effective for the patient’s specific condition.