In a world teeming with the complexities of addiction, Suboxone emerges as a beacon of hope for many who tread the challenging path to recovery. Yet, a haze of myths clouds its true purpose and benefits. You might be grappling with the echoing question: does Suboxone get you high? It is a concern that many carry, but let’s embark on a myth-busting journey where the facts shine brighter than the falsehoods.
Dispelling Myths: Does Suboxone Get You High?
Suboxone is often enveloped in myths, chiefly due to its classification as a partial opioid agonist. We’re going to lay it out straight—Suboxone is primarily designed to combat opioid dependence, supporting those in the embrace of recovery. Yet, whispers persist, suggesting that Suboxone might induce euphoria. To cut to the chase, for individuals not accustomed to taking opioids, Suboxone can potentially produce a mild high, but for those who are opioid-dependent, it’s a different story. The truth lies in the science of its makeup, which prioritizes healing over high.

Suboxone’s Composition and Purpose
Unlocking the puzzle of Suboxone starts with its ingredients: buprenorphine and naloxone. It’s a one-two punch that curtails cravings and nullifies the highs. Buprenorphine is the leading man here, offering relief without the full throttle of a traditional opioid. Naloxone waits in the wings, ready to step up if Suboxone’s course is diverted from its intended use. It’s critical to underscore that when taken as prescribed, Suboxone doesn’t dish out the same euphoric rush as its opioid cousins. Instead, it’s a lifeline back to sobriety.
| Aspect | Details |
| Product Name | Suboxone |
| Active Ingredients | Buprenorphine (partial opioid agonist) and Naloxone (opioid antagonist) |
| Intended Use | Medication-assisted treatment for opioid dependence; to reduce withdrawal symptoms and cravings |
| Possible Euphoric Effect | Limited due to the ‘ceiling effect’ of buprenorphine at moderate doses, designed to prevent a significant high |
| Abuse Potential | Lower than full agonist opioids, but still present, especially when injected or taken inappropriately |
| Naloxone Function | Added to deter intravenous abuse; precipitates withdrawal symptoms in opioid-dependent individuals |
| Prescribed Form | Sublingual tablets or film |
| Common Side Effects | Nausea, headache, constipation, sweating, insomnia, etc. |
| Misuse Outcomes | Respiratory depression (rare at prescribed doses), potential overdose when combined with other depressants |
| Functional Benefits (when used appropriately) | Reduces illicit opioid use, lowers risk of overdose, improves social functioning |
| Cost | Can vary widely; often covered by insurance plans or patient assistance programs |
| Prescription Required | Yes, classified as a Schedule III controlled substance by the DEA |
| Regular Monitoring | Recommended to mitigate risks of misuse and dependence |
| Alternative Therapies | Methadone, naltrexone |
The Role of Buprenorphine in Suboxone Treatment
Buprenorphine’s claim to fame is its ceiling effect—basically, after a certain point, taking more won’t heighten the effect, contrary to opioids like heroin. This cap not only curtails the risk of abuse but makes it a safer bet, especially considering the lower odds of respiratory depression. In essence, buprenorphine is the steady hand guiding individuals through withdrawal without tipping them over the edge.

Naloxone: The Protective Agent in Suboxone
Playing defense, naloxone swoops in to block opioid receptors, yanking away any ideas of misuse. If someone tries to game the system by injecting Suboxone, naloxone has their number, triggering withdrawal symptoms instead. By examining how naloxone operates within Suboxone, we appreciate its role in bolstering the medication’s abuse-deterrent armor. It’s a true example of how collateral efforts ensure the primary mission’s success.
User Experiences with Suboxone: High or Relief?
Let’s huddle around the campfire of firsthand experiences, where tales from those who’ve walked the walk talk louder than any textbook. The consensus swings more towards relief than any high-flying adventure. Notwithstanding, these narratives also serve as a stark reminder that every journey is deeply personal, and the effects can vary.
Can You Overdose on Suboxone?
A conversation about opioids without addressing the overdose elephant in the room? Unthinkable. So, to tackle the big question: can you overdose on Suboxone? Overdose risks are real yet mitigated when Suboxone is used responsibly. In the landscape of harm reduction, Suboxone takes a stand, showcasing a significant reduction in overdose incidents relative to other opioids when wielded correctly.
Suboxone in the Bigger Picture of Opioid Addiction Treatment
It’s time to widen our lens and plop Suboxone in the thick of opioid addiction treatments. We’ll cross-examine it against alternatives like methadone and wrap our heads around the nuances of each option. The data doesn’t lie—Suboxone has etched its place in addiction medicine as an effective intervention, not only in clinical trials but echoed in the throes of real-world challenges.
Misuse and Abuse: Recognizing and Preventing Suboxone Diversion
Suboxone is not immune to the clutches of misuse and diversion. Understanding the why and how of this issue is pivotal, and we’ll shine a light on the safeguards employed to fend off these mishaps. It’s about harnessing education as the sword and community involvement as the shield to keep Suboxone in the hands of those it’s meant to heal.
Voices from the Field: Healthcare Provider Perspectives on Suboxone
Who better to consult than the healthcare warriors doling out Suboxone prescriptions with caring hands? Gleaning insights from these sentinels gives us a well-rounded view of Suboxone’s effectiveness and the sticky web of myths surrounding it. These perspectives add a rich layer of depth, bolstering our mission to understand and convey the truth about opioid addiction treatment.
Conclusion: Reframing the Conversation on Suboxone
In our parting words, let’s reshape the chatter on Suboxone, embracing it as a cornerstone of recovery over a misunderstood substance prone to abuse. Through illuminating discussions and heartfelt education, we stand to redefine the narrative of opioid dependence treatment. By busting myths and championing truths, we hope to arm you with knowledge and foster a community of understanding, one where Suboxone is seen as a stepsister to sobriety, not a key to recreational highs.
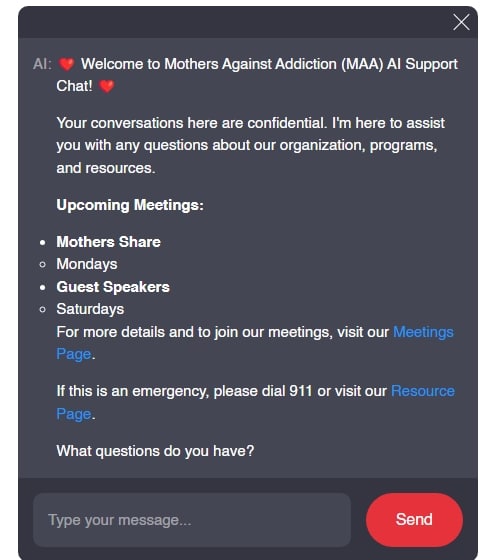
In every word of this article, we’ve woven the threads of factual data, scientific insights, and heartfelt stories to offer a tapestry that resonates authenticity and hope. From demystifying misconceptions to delving into real-world applications, our goal has been to craft a narrative that informs, supports, and empowers. There is beauty in the truth, and power in knowledge—this is the credo of MothersAgainstAddiction.org, and as we stand united in the battle against addiction, let’s carry these torches of clarity and compassion into the future.
Does Suboxone Get You High? Myths Debunked
When discussing whether Suboxone can get someone high, let’s talk turkey: the medication is specifically designed to combat opioid addiction, not to give you a buzz. However, misconceptions fly around like leaves in a tornado. One common myth is that Suboxone is just a “legal high,” which is as far-fetched as thinking the walk hard cast could provide you with a medical degree. The reality is, Suboxone is a combination of two medications—buprenorphine and naloxone—and is used to manage opioid dependence. Buprenorphine contributes to the effectiveness of Suboxone, and while it’s a partial opioid agonist, meaning it can produce similar effects to opioids, it’s like comparing a moped to a motorcycle when it comes to the “high” it can induce.
Now, imagine you’re at a Gamestop black friday 2024 sale, adrenaline pumping, driven by the thrill of the deal—that rush isn’t too far off from how someone might inaccurately imagine the effects of Suboxone. But, in truth, when taken as prescribed, the medication should not cause a significant euphoria. It’s more like listening to the soothing melodies of the love on tour final Shows, which calms you without overstimulation. To make sure you’re on the right track, look out for the Signs Suboxone dose Is too low, as they can give you a clear indication if your treatment is not optimized.
Switching lanes a bit, let’s consider how long the medication stays in the spotlight—similar to how one might ponder How long Does Suboxone stay in Your system. Both buprenorphine and naloxone have different half-lives, which means they hang around in your body for varying lengths of time, but not indefinitely—much like how Puedo ir al Bano isn’t a statement that will make sense at any point of a Spanish conversation. It’s crucial to understand the differences between Buprenorphine Vs Suboxone, as buprenorphine on its own can be detected in a Bup drug test, while Suboxone, with its mix of ingredients, may require more specific testing to identify.
So, while the theater of recovery casts a wide net of treatments and medications, it’s crucial to distinguish between fact and fiction—just like knowing whether can You snort xanax is a script for disaster rather than a line of treatment. Remember, the key to using Suboxone effectively is not about reaching for the stars but rather keeping your feet firmly on the ground, supported by solid, evidence-based medical advice.