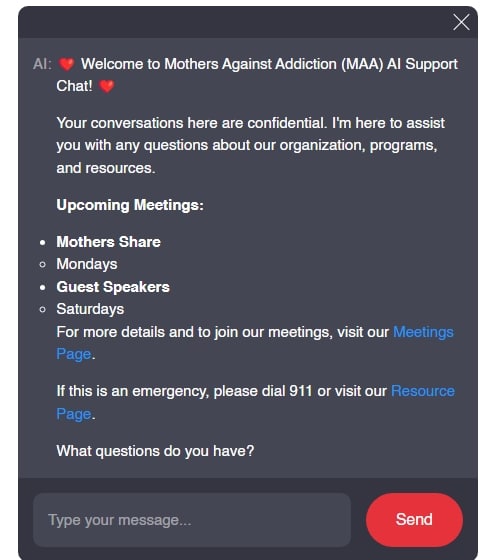
In the journey of overcoming opioid use disorder (OUD), understanding the various treatment options is crucial for families grappling with this challenge. Mothers Against Addiction stands as a beacon of hope for parents watching their children struggle with addiction or mourning the loss of a loved one to this crisis. We embark on an insightful exploration of two key medications in the MAT (Medication-Assisted Treatment) arsenal: Buprenorphine vs Suboxone. Through empathy and resilience, we unravel their roles, effectiveness, and safety, guiding you toward the most informed choices for healing and recovery.
Unveiling the Differences: Buprenorphine vs Suboxone for Safer Healing

Exploring the Core: Understanding Buprenorphine and Suboxone
Opioid addiction has woven a complex history of struggle and relief through various treatments, culminating in innovations like MAT. At the heart lie buprenorphine and Suboxone, each a herald of hope but carrying distinctive features and outcomes.
Buprenorphine is a partial opioid agonist that blunts cravings and withdraws symptoms without the high associated with opioid abuse. Recognized for reducing the likelihood of overdose, it has gained prominence in the fight against OUD. Its notable safety profile is etched in its classification as a Schedule III substance, signaling a lower potential for abuse.
On the flip side, Suboxone marries buprenorphine with naloxone, an opioid antagonist. This dual-ingredient medication stands guard against misuse, as naloxone induces withdrawal symptoms when tampered with, reinforcing its role in curbing addiction.
The stigma surrounding OUD often overshadows the effectiveness of these treatments. Understanding how each medication functions is imperative to not only treat but also accept OUD as a chronic yet manageable condition.
| Feature | Buprenorphine | Suboxone (Buprenorphine/Naloxone) |
|---|---|---|
| Primary Use | Treat opioid dependence and moderate-to-severe pain | Treat opioid addiction as part of a complete treatment program |
| Components | Only buprenorphine | Combination of buprenorphine and naloxone |
| Mechanism of Action | Partial opioid agonist | Partial opioid agonist (buprenorphine); opioid antagonist (naloxone) |
| Intended Outcome | Diminish withdrawal symptoms and cravings; manage pain | Diminish withdrawal symptoms and cravings; prevent misuse |
| Prescription Classification | Schedule III substance (lower potential for abuse) | Schedule III substance (lower potential for abuse) |
| Effect on Overdose Safety | Increased safety due to ceiling effect on respiratory depression | Increased safety due to naloxone, which counters opioid effects during overdose |
| Risk of Misuse | Lower potential relative to full agonists like methadone | Even lower potential due to presence of naloxone which precipitates withdrawal when injected |
| Formulations | Tablet, film, implant, injection | Sublingual tablet, sublingual film |
| Treatment for Pain | Yes, in specific formulations | No, not indicated for pain treatment |
| Additional Considerations | May be preferable in cases where naloxone is contraindicated or for pain management | Contains naloxone to discourage intravenous misuse |
| Counseling and Therapy | Recommended as part of a comprehensive treatment plan | Strongly advised as part of a complete treatment program |
| Cost | Varies by formulation and insurance coverage | Varies by formulation and insurance coverage; generally similar to buprenorphine |
Belbuca vs Suboxone: The Battleground of Efficacy and Safety
When pondering Belbuca vs Suboxone, we delve into specifics. Belbuca, delivering buprenorphine through a buccal film, targets chronic pain management, unlike Suboxone, which is tailored to combat OUD.
Suboxone steps forward with a user-friendly sublingual film delivery method. Its intended phase is the maintenance of OUD recovery, catering to the needs of individuals seeking to break free from opioid dependence.
Our comparative lens scrutinizes absorption rates, potency, side effects, and safety. Case studies paint a vivid picture, allowing us to learn from those who have walked this path before, finding solace in either Belbuca’s focused approach or Suboxone’s comprehensive shield.

Comprehensive Comparison: Buprenorphine vs Suboxone in OUD Recovery
Choosing between isolated buprenorphine and Suboxone isn’t a matter of mere preference but an assessment of an individual’s unique situation. For some, the singular focus of buprenorphine on easing withdrawal and cravings suffices, offering a less complex treatment path.
Nevertheless, the dual dynamics of Suboxone—the presence of naloxone—bring a fortified layer against relapse. Healthcare providers weigh factors like patient history, risk of diversion, and potential for relapse when deciding which medication to prescribe.
Regulations and legal constraints are pivotal in this equation, as accessibility to each medication can tilt the scales, leaving healthcare providers and patients to navigate a labyrinth of rules.
Painting the Full Picture: Subutex vs Suboxone in Patient Treatment Plans
Distinguishing Subutex from Suboxone is simple on the surface—Subutex contains buprenorphine alone. But, when we peer below, we see Subutex’s narrowed use in initial phases of detox, while Suboxone’s realm is maintenance.
Our line-by-line showdown reveals that while Subutex can be a starting line, Suboxone often becomes the marathon runner, replete with psychological and withdrawal advantages nestled within its dual components, aligning well with harm reduction strategies.
Patient stories offer a nuanced view, uncovering the divergent reactions and successes with both medications—each story a thread in the broader tapestry of OUD recovery.
Perspectives from the Field: Expert Opinions on Buprenorphine vs Suboxone
Venturing further, we seek wisdom from the frontlines. Medical professionals dedicated to addiction treatment share their candid perspectives, corroborating our findings with empirical knowledge.
Patient surveys and testimonials add depth, personalizing the narrative of buprenorphine vs Suboxone. They become more than just names; they represent lifelines to many in the throes of recovery.
Prescribing trends and their resultant impact on recovery underscore a dynamic field ever in flux, the symbiosis between counseling, and psychosocial support with MAT undeniably pivotal in successful outcomes.
Scrutinizing Side Effects: How Buprenorphine and Suboxone Compare
Like all medicines, buprenorphine and Suboxone carry the baggage of side effects. We dissect these, addressing the long-term ramifications on physical and mental well-being, separating fact from fiction.
Addressing myths head-on, we dispel fears, spotlighting strategies to mitigate adverse effects and preaching the gospel of informed, empowered patient education.
Balancing Costs: Economic Considerations in Buprenorphine vs Suboxone Treatment
The economic lens reveals a stark reality—the price tag of healthcare can’t be ignored. We analyze cost-effectiveness, insurance nuances, and the broader impact on the economy, illuminated through real-life case studies.
The story emerges of proactive mitigation of economic strain through effective MAT, buprenorphine, and Suboxone becoming not only health saviors but also financial alleviators in communities riddled with OUD.
Navigating the Journey Forward: Advancements and Innovations in MAT
Peering into the horizon, we celebrate advancements in MAT, buprenorphine, and Suboxone formulations leading the charge. Research paves new roads toward overcoming OUD, with technology’s hand evident in treatment adherence and monitoring.
Policies evolve, forming the backdrop against which new treatments emerge, shaping the choices and access that will define tomorrow’s recovery journey.
Conclusion: Charting a Safer Path in OUD Treatment
With the tapestry of buprenorphine vs Suboxone woven before us, we arrive at a point of introspection and vision. Recommendations crystallize for practitioners, policymakers, and families, all players in the grand scheme of recovery.
A brighter future of MAT beckons—one accentuated by compassion, innovation, and open arms. The imperative is clear: ongoing education, the dispersion of stigma, and unwavering support for the recovery community will chart the path to a safer tomorrow.
This haven of knowledge and support serves as your companion on the road less traveled, the journey of recovery from the grasp of opioid addiction. At Mothers Against Addiction, we walk this path with you, anchored in the belief that understanding fosters safety, and knowledge is the beacon guiding us to the gentle shores of healing.
Buprenorphine vs Suboxone: Which Heals Safer?
The Breakdown: What’s the Difference?
Ah, the conundrum of buprenorphine vs Suboxone—sounds like a heavyweight bout, doesn’t it? But really, it’s like comparing a cozy hotel pillow to the entire room—it’s just part of the bigger picture. Let’s get this straight: Suboxone has buprenorphine in it, along with a dash of naloxone to deter abuse, kind of like how adding a portable sink enhances outdoor events by bringing a slice of home convenience.
Well now, you may wonder, “Can buprenorphine fly solo?” Sure can! And it often does, playing a pivotal role in addiction treatment. But if you’re cleverly trying to beat a Bup drug test, think twice. Because buprenorphine is like that one unforgettable guest at a party in Dunkirk, NY—it leaves a mark, and people will remember it’s been there.
Picking What’s Right: Not a High Stakes Game
Now, if you’re on the recovery road and thinking, Does Suboxone get You high? you’re not alone. But fret not—Suboxone is designed to side-step the high and steer the ship towards calmer waters. It’s more about stability and less about thrill, quite the opposite of, say, flipping through scandalous Meghan Markle nude headlines.
Speaking of too much of a good thing, keep an eye out for Signs Suboxone dose Is too low. Because, honestly, who wants to feel like they’re showing up to a winter party in Dunkirk, NY without a coat? It’s important to stay wrapped up in that just-right dose, making sure your recovery journey is snug as a bug.
Lingering Guest: How Long Does It Stay?
Okay, but how long does Suboxone hang around, you ask? Imagine Suboxone as a cousin who crashed on your couch after a wild family reunion; that’s how How long Does Suboxone stay in Your system feels sometimes. It could be a few days, or it might feel like an eternity before they pack up their Nuded Boobs shirts and hit the road. The takeaway? A Suboxone stint can stay in the system, peeking out like a shirt tag, longer than expected. But no worries; it’s all part of the healing hug that Suboxone gives on its way out.

Is Suboxone same as buprenorphine?
– Hold up, don’t get ’em twisted! Suboxone ain’t the same as buprenorphine. Suboxone is like a duo, packing both buprenorphine and naloxone. In contrast, buprenorphine flies solo, sans naloxone. The combo in Suboxone has got your back to keep opioid dependency at bay.
Is buprenorphine patch the same as Suboxone?
– Nah, the buprenorphine patch and Suboxone are cousins, not twins! The patch sticks to you, delivering buprenorphine only, while Suboxone slips under the tongue and brings naloxone into the mix for that one-two punch against opioid addiction.
Why is buprenorphine preferred?
– So, here’s the scoop on buprenorphine – folks dig it ’cause it’s a bit of a softie for an opioid, meaning it’s tougher to abuse and easier on your system if you take too much. Plus, it eases off the withdrawal and cravings, which is a big win when you’re battling the beast of opioid dependency.
Is buprenorphine and naloxone sublingual film the same as Suboxone?
– Alrighty, let’s clear this up: buprenorphine and naloxone sublingual film is indeed Suboxone. They’re one and the same, the perfect tag team of meds used in the smackdown against opioid addiction.
Why is Suboxone being discontinued?
– Whoa there, hold your horses! No, Suboxone isn’t getting the boot—they haven’t pulled the plug on this lifesaver. It’s still out there fighting the good fight as part of addiction treatment.
Is buprenorphine generic for Suboxone?
– Yup, generic alert! Buprenorphine’s the main event in Suboxone, playing the lead role without the fancy brand name and the naloxone sidekick in its solo versions.
Is a buprenorphine patch a narcotic?
– Is a buprenorphine patch a narcotic? You betcha, it’s an opioid, which is in the narcotic family. But it’s got a special talent for playing nice with fewer cravings and less risk if you go overboard.
What kind of pain does buprenorphine treat?
– Buprenorphine’s a jack-of-all-trades, taking on moderate-to-severe pain without breaking a sweat. But remember, that’s when it’s riding solo, not when it’s paired up with naloxone in Suboxone.
How many mg of buprenorphine for pain?
– How much buprenorphine for pain, you ask? It’s all about striking a balance—doses vary, but they’re usually kept on the down low to kick pain to the curb without inviting trouble.
Is tramadol the same as buprenorphine?
– Don’t get bamboozled—tramadol and buprenorphine aren’t even in the same league. Tramadol’s a painkiller, sure, but buprenorphine’s got that special touch for addiction treatment and plays hardball with pain too.
What to avoid when taking buprenorphine?
– When you’re teaming up with buprenorphine, remember it’s a no-go for booze, sedatives, or other opioids. Mixing those can turn real ugly, real fast—it’s a cocktail you don’t want to mess with.
Why do doctors prescribe buprenorphine for pain?
– Docs turn to buprenorphine for pain ’cause it’s like a bouncer at a club—it’s tough on pain but plays nice, keeping the risk of dependence and side effects lower than some of the heavy hitters out there.
What is the strongest Suboxone?
– The strongest Suboxone around? That’d be the heavyweight champ, Suboxone 12 mg/3 mg. It packs the mightiest buprenorphine and naloxone combo punch for keeping opioid addiction on the ropes.
Is it OK to cut Suboxone film in half?
– Can you slice Suboxone film in half? Sure thing! If your doc gives you the green light, you can cut it to get the dose that fits you like a glove. Just make sure you’re sharp about following their game plan.
Is there a lawsuit against Suboxone?
– Litigation lowdown: Yes, there’s been legal rumbling against Suboxone makers for their business moves, but it’s all about the dollars, not the drug’s safety or effectiveness in the ring of addiction treatment.
What is the generic name for buprenorphine?
– The generic name for buprenorphine? It’s simply ‘buprenorphine.’ No frills, no thrills, just the plain old molecule ready to roll up its sleeves and get down to business.
What is a substitute for buprenorphine?
– On the hunt for a buprenorphine substitute? Your options may include other medications like methadone or naltrexone. They’re from the same gang, tackling addiction, but each has its own way of setting things straight.
What are the two types of Suboxone?
– The two types of Suboxone? You’ve got the Suboxone sublingual film and the tablet, both ready to rumble with buprenorphine and naloxone in their corner, tag-teaming against opioid addiction.
What is the other name for buprenorphine?
– Another name for buprenorphine? Well, it’s often called by its street names like “bupe,” “subs,” or “orange guys,” but in the clinic, they’ll stick to buprenorphine or its trade names, no matter the chitchat.