In the shadows of our society lurks an often-overlooked menace: the intersection of eating disorders and addiction. This dark interplay silently wreaks havoc on countless lives, yet remains under-discussed. Understanding the complex relationship between these two conditions is crucial for parents striving to help their children fight addiction or grappling with the loss of a child to these dual adversities.
The Dark Interplay Between Eating Disorders and Addiction
Eating disorders and addiction are twin specters haunting nearly every corner of the world, feeding off each other in a relentless cycle. While the public is somewhat aware of anorexia and substance abuse as separate entities, the brutal truth about their interconnected nature seldom comes to light. The combined force of these issues complicates recovery, making each step toward sobriety more challenging.
The synergy between eating disorders and addiction doesn’t merely double the trouble; it creates an insidious loop that proves difficult to break. The path to recovery demands a detailed understanding of how these conditions reinforce each other and the need for holistic intervention.
The Biology of Both Disorders: A Shared Genetic Predisposition
Emerging research unveils a striking genetic overlap between eating disorders and addiction. Studies from the National Institute on Drug Abuse reveal that individuals with eating disorders often carry genetic markers associated with impulse control and reward-seeking behaviors—traits similarly found in those battling addiction.
This shared genetic groundwork suggests that both conditions stem from overlapping biological vulnerabilities. These genetic markers not only make individuals more susceptible to these disorders but also complicate the recovery process, necessitating a multifaceted approach to treatment.
| Aspect | Description |
| Prevalence | – Up to 50% of individuals with eating disorders use alcohol or illicit drugs, which is five times higher than the general population. – Up to 35% of individuals who were dependent on alcohol or other drugs also have eating disorders, which is 11 times greater than the general population. |
| Development Relationship | – Individuals experiencing disordered eating are more likely to develop substance use disorders than the reverse (Gregorowski et al., 2013). – Substance abuse may serve as a means to self-medicate negative feelings and emotions associated with eating disorders. |
| Health Impacts | Both eating disorders and addiction can seriously affect an individual’s ability to obtain necessary nutrition and can lead to various health issues including: – Heart-related issues – Digestive system problems – Bone weakness – Dental issues – Mental health issues like depression, anxiety, self-harm, and suicidal behaviors |
| Causes | Eating disorders have no single cause. They result from a complex combination of biological, psychological, and sociocultural factors that interact with genetic vulnerabilities. |
| Coping Mechanisms | Individuals with eating disorders typically exhibit deficits in coping strategies. Disordered eating behaviors may act as maladaptive coping mechanisms (e.g., binge eating or extreme food restriction to cope with negative emotions). |
| Comorbid Conditions | Eating disorders are commonly linked with several comorbid psychological conditions such as: – Depression – Anxiety disorders – Self-harm tendencies – Suicidal thoughts and behaviors |
| Impact on Daily Life | – Extreme food restriction or binge eating can interfere with daily activities and social interactions. – Substance use alongside disordered eating exacerbates these functional impairments. |
| Statistics Source | – Gregorowski et al., 2013 – The National Center on Addiction and Substance Abuse – Various clinical observations and studies (cited up to March 28, 2023) |
The Vicious Cycle: How One Disorder Fuels the Other
Real-life stories illustrate the vicious cycle between eating disorders and addiction. Take the singer and activist Demi Lovato, for example. Her very public battles with both conditions shed light on how one disorder can exacerbate the other. Lovato’s struggle with substances often aggravated her tendencies toward disordered eating, and vice versa. This interplay forms a cycle where each condition reinforces the other, making it hard to achieve long-term recovery.
Understanding these interdependencies can illuminate pathways for more effective treatment strategies. Addressing the root causes of both conditions simultaneously is essential for breaking this vicious cycle.
Underreporting and Misdiagnosis: The Invisible Epidemic
Diagnosing and treating individuals grappling with both eating disorders and addiction pose unique challenges. Health professionals often underreport these co-occurring disorders due to prevalent shame and stigma. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), this leads to misdiagnoses and inadequate treatment protocols.
Many patients hesitate to disclose their struggles with two stigmatized conditions, fearing judgment or misunderstanding. Consequently, effective treatment often remains out of reach, perpetuating a cycle of suffering that affects not just the individuals, but their families as well.
Comprehensive Treatment Plans: Bridging Two Worlds
Addressing both disorders simultaneously requires innovative and integrative treatment models. Institutions such as the Hazelden Betty Ford Foundation are pioneering approaches that combine therapy modalities like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT). These methods are tuned to tackle both addiction and disordered eating behaviors concurrently.
Such comprehensive plans are essential for effective intervention, as they bridge the gap between two traditionally separate treatment worlds. By treating the whole person rather than just the symptoms, these integrative approaches hold promise for sustainable recovery.
The Role of Families and Support Systems: The Unsung Heroes
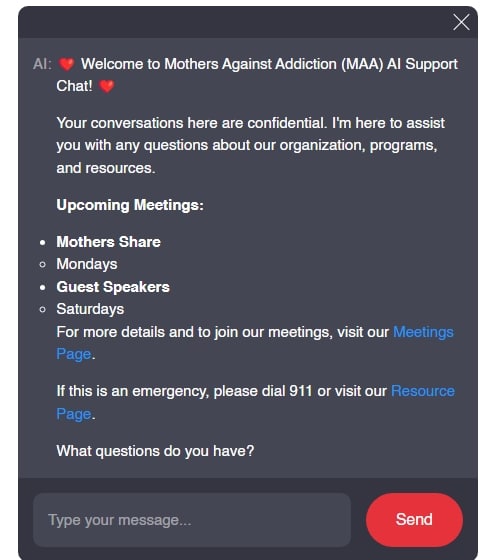
In the fight against eating disorders and addiction, families are the unsung heroes. They often serve as the frontline defense, providing support systems that are both steadfast and compassionate. Organizations like Mothers Against Addiction offer valuable resources to help parents navigate this intricate web of challenges. Parental advocacy, unwavering support, and timely intervention can significantly reshape the recovery journey.
Family involvement can dramatically improve recovery outcomes. It’s essential for parents to stay informed, active, and supportive throughout the recovery process. This trio of family support can tilt the scales towards successful and lasting recovery.
Raising Awareness: Tackling Stigma and Misconceptions
Raising awareness and dismantling stigma around eating disorders and addiction is crucial. Nonprofits like Project HEAL spearhead public campaigns focusing on these dual conditions. Their social media efforts play a vital role in de-stigmatizing these co-occurring disorders, encouraging more individuals to seek help without fear of judgment.
Awareness drives aim to challenge misconceptions and highlight the need for understanding and empathy. Through education and advocacy, we can create a more supportive environment for those affected, promoting a cultural shift in how we approach these issues.
Innovative Approaches and Future Research: The Path Forward
Ongoing research and innovative therapies are essential for effectively addressing co-occurring disorders. Neurofeedback therapy, for instance, shows promise in treating both addiction and eating disorders. This technique involves real-time monitoring of brain activity to guide patients through exercises that promote healthier brain function.
Continuous research into new therapies and treatments is imperative for developing strategies that offer holistic and sustainable recovery solutions. As our understanding of these disorders evolves, so too must our approaches to treatment and care.
The Imperative for Holistic Healing
The intersection of eating disorders and addiction presents a formidable challenge necessitating nuanced understanding and multi-dimensional treatment approaches. Addressing these co-occurring disorders demands comprehensive strategies incorporating medical, psychological, and social support systems.
By fostering a deeper recognition of how these conditions intertwine, we can better support those grappling with this hidden crisis. Holistic healing holds the key to sustained recovery, emphasizing that complete recovery extends beyond merely treating symptoms. It’s about reclaiming lives and fostering resilience amid adversity.
For more resources on stress management techniques, visit Mothers Against addiction.
At Mothers Against Addiction, we stand by parents facing the heart-wrenching reality of their child’s struggle with addiction or enduring the unthinkable pain of loss. Through understanding, advocacy, and comprehensive support, we strive to uncover the hidden crisis of eating disorders and addiction—empowering families every step of the way.
Eating Disorders and Addiction’s Hidden Crisis
Commonalities and Overlaps
Did you know that eating disorders and addiction often go hand-in-hand? These conditions share many underlying factors such as genetic predisposition, neurochemical imbalances, and emotional distress. Indeed, individuals suffering from either disorder frequently struggle with emotional regulation in recovery, which can make overcoming both challenges incredibly tough.
The Silent Epidemic
It’s astonishing how intertwined these issues can be, yet they often fly under the radar. For instance, many people turn to substance use to cope with the overwhelming emotions associated with an eating disorder. Understanding the latter define these crises not just as separate but as interconnected can be a game-changer in providing effective treatment.
The Toll on Mental Health
Another sobering fact is the increased risk of suicide among individuals struggling with both eating disorders and addiction. Undoubtedly, this brings an urgent need for comprehensive suicide prevention strategies, to help those at risk find a way out of their dual struggle. The intertwining issues can create a perfect storm, leading to tragic outcomes if not addressed holistically.
The Cost of Recovery
Financial strain is another hidden crisis. The most affordable options for treatment might not always be the best fit for everyone. Similar to how building the Cheapest Homes To build might save money up-front but result in higher long-term costs, opting for the least expensive treatment option could mean higher emotional and financial costs down the road. Effective treatment often demands significant investment, and finding affordable yet comprehensive options is crucial.
Everyday Life Impact
These issues can subtly invade everyday life. Just think about how a trip to a delightful patisserie Poupon can turn into a battlefield for someone grappling with both addiction and an eating disorder. It’s more than just a casual indulgence; it’s a fight against urges and habits that can spiral out of control.
Understanding these interconnected crises can shed light on the full spectrum of challenges faced by those struggling with eating disorders and addiction. The more we learn, the better equipped we are to provide the support and solutions needed to truly make a difference.
Can eating disorders lead to drug addiction?
Yep, eating disorders can lead to drug addiction. Up to 50% of folks with eating disorders also use alcohol or illicit drugs, which is way higher than the general population. The relationship goes both ways, but disordered eating often precedes the substance use.
How does having an eating disorder affect your life?
Having an eating disorder can seriously mess with your life. It affects your heart, digestive system, bones, teeth, and mouth. Plus, it can lead to other health problems and is often tied to depression, anxiety, self-harm, and suicidal thoughts.
What is the biggest cause of an eating disorder?
There’s no single cause for an eating disorder. It’s a mix of biological, psychological, and sociocultural factors that come together. Some people have a genetic vulnerability that gets triggered by these factors.
Is an eating disorder a coping mechanism?
Eating disorders can be seen as a coping mechanism. Folks with these disorders often have trouble dealing with stress or negative emotions, and they might turn to disordered eating behaviors like binge eating or extreme food restriction to cope.
What disorders are associated with addiction?
Addiction is often seen alongside disorders like depression, anxiety, and eating disorders. A person’s attempt to self-medicate negative feelings can lead to the use of alcohol or drugs.
Which eating disorder has the most common relapse?
Bulimia nervosa often has the most common relapse. It’s a tough cycle to break because the patterns of bingeing and purging can be deeply ingrained and hard to stop.
How do people with eating disorders behave?
People with eating disorders might be secretive, obsessed with food, weight, or body image, and engage in extreme behaviors like binge eating, purging, or excessive exercising. They might also avoid social situations involving food.
Do people with eating disorders know they have a problem?
Not everyone with an eating disorder knows they have a problem. Sometimes there’s denial or a lack of awareness of the seriousness of the issue. They might justify their behaviors as normal or necessary.
What happens to your mind when you have an eating disorder?
When you have an eating disorder, your mind is often preoccupied with thoughts about food, weight, and body image. It can lead to distorted thinking, obsessive behaviors, and a lot of stress and anxiety.
What triggers eating disorders?
Triggers for eating disorders can include traumatic events, societal pressure, negative body image, and sometimes, family history. Even things like major life changes or personal stress can set them off.
What type of person develops an eating disorder?
Anyone can develop an eating disorder, but it often starts during the teenage years. People with perfectionist tendencies, low self-esteem, or those experiencing high levels of stress or trauma are more at risk.
How to fix eating disorders?
Fixing eating disorders usually involves a team approach, including medical treatment, nutritional counseling, and therapy. It’s important to address both the physical and psychological aspects of the disorder.
Are eating disorders a trauma response?
Eating disorders can be a response to trauma, as people might use disordered eating behaviors to cope with the emotional pain. The relationship between trauma and eating disorders is complex and varies from person to person.
How do people with eating disorders feel about themselves?
People with eating disorders often feel a lot of guilt, shame, and low self-esteem. They might have a distorted view of their body and a relentless fear of gaining weight, leading to a constant struggle with their self-worth.
What not to say to someone with an eating disorder?
Avoid saying things that focus on appearance or dismiss the seriousness of the disorder. Phrases like “just eat more” or “I wish I had your problem” can be very harmful. It’s better to express support and encourage them to seek professional help.
Is there a link between mental illness and drug addiction?
There’s definitely a link between mental illness and drug addiction. Disorders like anxiety, depression, and eating disorders often co-occur with substance abuse, as people might use drugs or alcohol to cope with their symptoms.
Can eating become an addiction?
Yes, eating can become an addiction. Similar to drug addiction, people might use food as a way to deal with emotional issues, and it can lead to compulsive behaviors around eating.
Why does abuse lead to eating disorders?
Abuse can lead to eating disorders because the trauma and emotional distress from abuse might drive people to control their eating as a way to cope. The feelings of powerlessness and low self-esteem from abuse can manifest in disordered eating behaviors.
Are addictive disorders genetic?
Addictive disorders, including eating disorders, can have a genetic component. If addiction runs in the family, there’s a higher risk that it might develop in other family members as well.