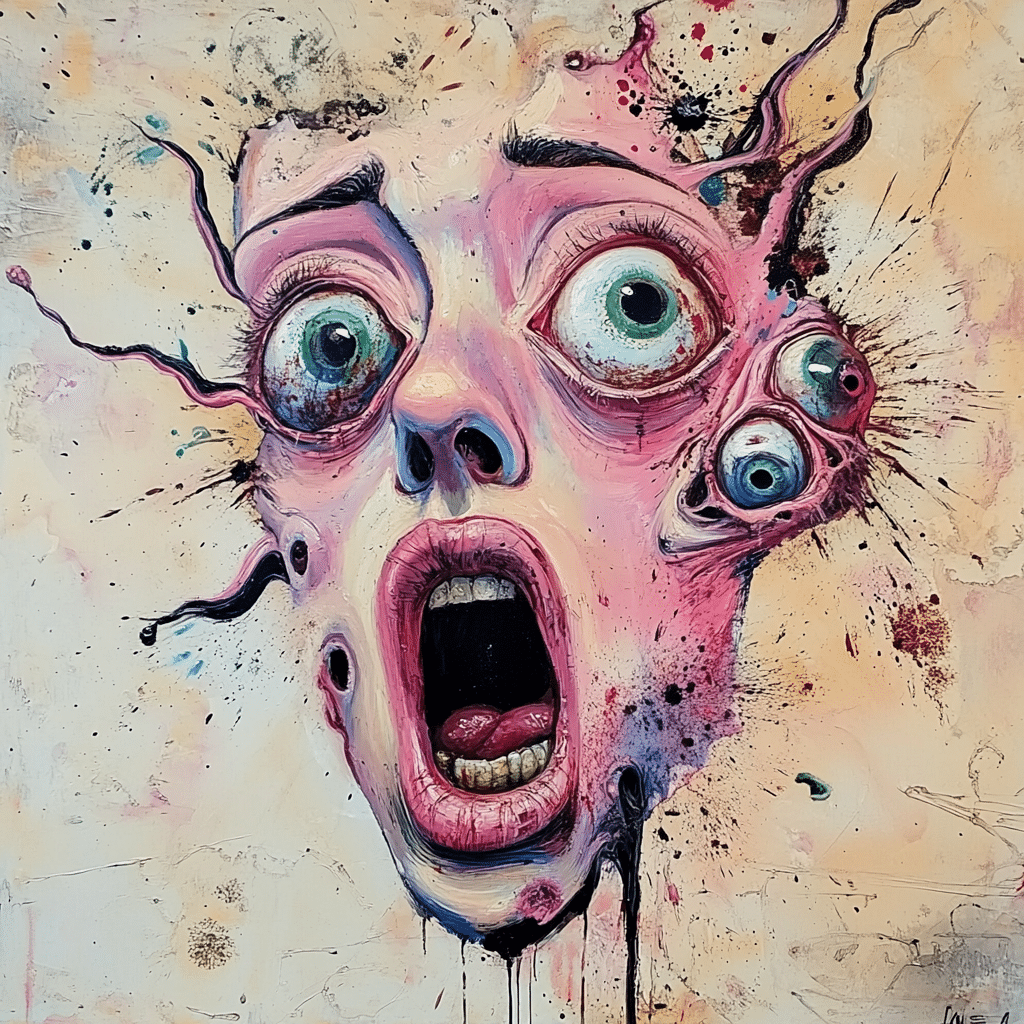
Psycosis is often like an unwanted guest at the worst time, sneaking in and wreaking havoc on individuals already battling the demons of addiction. This disconnection from reality manifests through troubling symptoms such as hallucinations and delusions. It’s vital to recognize that psychosis doesn’t just stem from mental health disorders like schizophrenia; it increasingly intertwines with addiction, particularly opioids. Parents watching their children spiral into the grips of opioid addiction can feel the weight of both helplessness and heartache as they confront the startling reality of psychosis alongside addiction. Understanding these challenges is crucial to creating a supportive community that fosters recovery.

Understanding Psycosis and Its Relationship with Opioids
When opioids like Oxycodone hydrochloride are involved, psycosis can emerge in ways that leave families grappling with fear and confusion. These powerful substances significantly change brain chemistry, leading to unsettling shifts in thought patterns and behaviors. Chronic opioid use can cause lasting alterations in neurotransmitter function, triggering symptoms of psychosis in individuals. This relationship underscores the importance of awareness among parents who see their children exhibiting erratic behaviors or slipping away into a world of delusions fueled by opioid dependency.
Parents might not be aware that withdrawal can also pave the way for psychosis. As an individual detoxes from opioids, the experience often comes with severe withdrawal symptoms, including anxiety and agitation. In some desperate cases, hallucinations can also occur. Thus, it’s clear that dependency turns into a frightening mental health crisis, reminding us of the intricate connection between addiction and psychosis.
The interplay doesn’t stop there. Research shows that individuals with pre-existing conditions, such as anxiety or depression, are at higher risk for experiencing psychosis while using opioids. A 2023 study revealed a staggering 40% increase in psychotic symptoms among those facing dual diagnoses. Understanding this connection equips parents with the knowledge to address their child’s needs holistically, fostering a more supportive approach to treatment.

5 Ways Opioids Initiate or Exacerbate Psycosis
Opioids disrupt the delicate balance of neurotransmitters like dopamine, leading to mood regulation issues and a distorted perception. Chronic users often show significant changes in dopamine function, resulting in troubling psychotic symptoms. Recognizing the neurological implications is key for families trying to understand the link between opioid misuse and psychosis.
Detoxing from opioids is no walk in the park. The journey is riddled with severe withdrawal symptoms, including increased anxiety and panic attacks. In some cases, hallucinations can emerge, amplifying the distressing intersection of addiction and mental health crises, making the detox phase a dangerous time for users.
The presence of comorbid conditions amplifies the risk of experiencing psychosis in those using opioids. Research points to dual diagnosis individuals facing profound challenges, as an addiction to opioids can worsen these underlying mental health issues. For families, this means navigating an additional layer of complexity in their loved one’s treatment.
Life stressors are a huge factor when it comes to substance abuse. Issues like unemployment, trauma, or relational conflict often push individuals towards opioid use as a coping mechanism. These environmental triggers can initiate both addiction and episodes of psychosis, showcasing the tight grip they can have on mental health.
Genetics also play a role. Certain family histories may predispose individuals to react severely to opioids, leading to heightened instances of psychosis. Ongoing research into genetic markers aims to unravel the ties between addiction and psychiatric disorders, offering valuable insight into who may be at risk.
The Impact of Psycosis on Families and Communities
When psychosis strikes, the fallout affects far more than just the individual. Families become entangled in a web of stigma, confusion, and lack of support. Parents wrestle with feelings of shame and misunderstanding, often feeling isolated from a community that may not comprehend their struggles. This lack of understanding can create insurmountable barriers, leaving families without the essential resources they need.
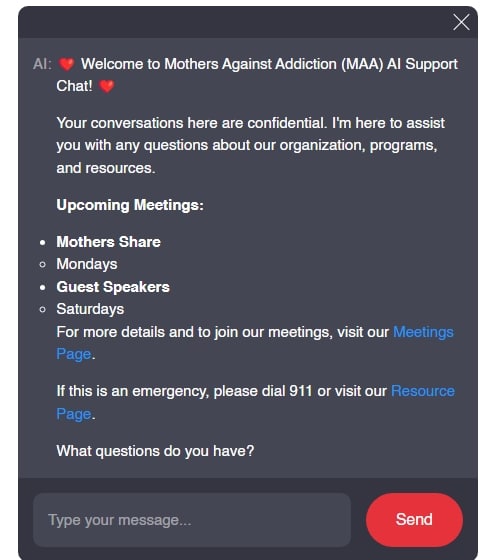
Navigating the healthcare system can be daunting. As parents face the reality of their child’s addiction and its connection to psychosis, they often do so without adequate understanding or access to treatment options. This highlights an urgent call for awareness and education about the interplay between mental health and substance abuse, emphasizing the necessity for resources like those offered through Mothers Against addiction.
Creating open and informed dialogues within our communities is a paramount step toward healing. The stories and struggles shared among families, whether in group settings or through online platforms, can create a sense of belonging. They remind us that no one is alone in this fight, painting a clearer picture of the need for support systems to be put in place.
Real-Life Stories of Struggle and Strength
One remarkable survival story comes from Emily, who faced a significant challenge in her battle against opioid addiction. Struggling with heroin addiction, Emily experienced bouts of severe paranoia and nightmarish auditory hallucinations. But with dedicated therapy that combined addiction recovery and psychiatric care, she carved a path to reclaim her life. Emily’s journey paints a hopeful picture, showing that with the right support, individuals can rise from the depths of both addiction and psychosis.
These testimonies are urgent reminders that recovery isn’t just about abstaining from substances; it’s about rebuilding lives. Many transformed individuals, including those in support groups facilitated by organizations like Mothers Against addiction, stress the importance of community support in recovery journeys. The emphasis on connecting with others fosters an environment of healing and resilience.
Through holistic treatment approaches, families can witness the metamorphosis that’s possible when individuals receive adequate care. Emily’s story, like many others, emphasizes the critical nature of comprehensive treatment, inspiring others to see beyond the struggles and celebrate victories, no matter how small.
The Road Ahead: Strategies for Holistic Healing
To effectively face the challenges presented by psychosis and opioid use, it’s time to embrace a multifaceted approach to treatment that doesn’t shy away from the complexities involved. Comprehensive treatment plans should encompass a blend of medication-assisted treatment (MAT), cognitive behavioral therapy (CBT), and family therapy.
When families become active participants in recovery, everyone benefits. Encouraging open discussions about mental health within addiction recovery promotes an environment where support networks can thrive. Providers should also recognize the critical role family dynamics play in shaping recovery outcomes, further pushing the need for collective treatment strategies.
Communities can unite in the fight against addiction and its vulnerabilities by advocating for broader systemic changes. Initiatives such as block Grants can pave the way toward better-informed resources, offering families the necessary tools to address both addiction and mental health with a comprehensive lens.
Building a Supportive Community
Cultivating a strong support community is essential for families touched by addiction. Nonprofits like Mothers Against addiction provide invaluable resources for parents, serving as beacons of hope. By advocating for systemic changes in addiction treatment, these organizations can help families find unity in their struggle.
Individuals are encouraged to engage in community discussions, lending their voices and experiences to help others understand the realities of addiction and psychosis. Connecting families with mental health professionals and establishing sponsorship opportunities can lead to meaningful change that resonates throughout entire communities.
Through a collective effort, the discussion surrounding psycosis needs to be elevated in conversations about mental health, policy-making, and community outreach. By developing a deeper understanding of this relationship, families can equip themselves with the necessary tools to confront challenges ahead, ensuring that the stories we hear don’t just echo struggles, but rather celebrate lives rebuilt and reclaimed.
In closing, the journey toward understanding psycosis and its ties to opioid addiction is fraught with challenges—yet with collective compassion and resilient action, we can turn the tide. By championing awareness and fostering supportive environments, we empower families to navigate their paths to healing, ensuring that like Emily, many more can emerge victorious.
Psycosis: The Hidden Struggles That Impact Lives
Understanding Psycosis and Its Reach
Psycosis can turn one’s life upside down, often leaving loved ones searching for answers. Surprisingly, around 3% of people will experience some form of psycosis in their lifetime. This mental health condition can manifest as hallucinations or delusions, leading individuals to see or hear things that aren’t real, which can be incredibly isolating. If you’ve ever felt the need for a good moisturizer to combat wrinkles while dealing with life’s stressors, you might relate; navigating such challenges can feel overwhelming. Finding the best facial moisturizer for aging skin can be just one way to take care of oneself while facing deeper issues like psycosis.
The Connection Between Psycosis and Medication
Many people dealing with psycosis may also be prescribed medications that can lead to side effects. For instance, some fear that changes in their weight, like experiencing lexapro weight gain, could impact their self-esteem or willingness to engage with the world. It’s a constant cycle of managing symptoms and addressing the repercussions of treatment. This struggle is often shared among families, many of whom turn to resources to cope with these challenges. One such resource is the Responder program, which offers support for anyone affected by addiction or mental health issues, allowing families to find guidance when dealing with psycosis.
Support Systems and Resources
Support systems can make all the difference for those dealing with psycosis. Community organizations and dedicated groups help to bridge the gap and provide necessary resources. Traveling to support meetings can feel like an adventure in its own right, especially when using a budget airline like Fronteir Airlines, which makes it more accessible for many families to connect and share their experiences. These gatherings foster understanding and allow individuals to feel less alone in their struggles with psycosis, providing a critical sense of belonging and support.
So while psycosis remains a challenging condition, awareness, support, and engagement can help alleviate its burdens. Engaging with resources like Responders, focusing on mental wellness, and maintaining personal care routines can empower individuals and their families to manage the effects of this often hidden struggle.