The issue of suicide by doctors has reached a tragic boiling point in the healthcare sector. This crisis deeply affects not only the physicians who succumb but also their colleagues, families, and the patients who rely on their care. Statistics show that physicians are over twice as likely to take their own lives compared to individuals in other professions, shedding light on an urgent issue we’re all responsible for addressing. In exploring the emotional toll of this epidemic, we uncover how we can all support healthcare workers struggling with their mental well-being.
Understanding the Tragic Impact of Suicide by Doctors
Suicide by doctors doesn’t just vanish in isolation; it creates a ripple effect throughout the healthcare ecosystem. When a physician dies by suicide, the emotional impact can be devastating. Colleagues may experience heightened anxiety, guilt, and feelings of inadequacy, which only serves to increase stress in a field that’s already rife with pressure. When multiple healthcare professionals are caught in this cycle, the quality of patient care invariably suffers as well.
The side effects of this silent epidemic run deep. Family members left behind often grapple with unimaginable grief while questioning what they could have done to prevent their loved one’s death. The patients who trusted their doctors experience confusion and betrayal when a trusted caregiver disappears. Communities may even face a healthcare worker shortage that exacerbates the issues of access to care, affecting everyone.
This silent crisis emphasizes the need for change. Identifying the systemic issues contributing to this epidemic is crucial, as it provides a foundation for solutions. When we shed light on the hidden corners of healthcare, we pave the way for open conversations that can serve as lifelines for struggling professionals.

Top 7 Contributing Factors to Suicide by Doctors
As we unravel the reasons behind suicide by doctors, several key factors emerge:
With over 60% of physicians reporting severe burnout, it’s no wonder our doctors feel overwhelmed. Long hours, endless patient loads, and high-stakes decisions can leave even the most resilient professionals feeling lost and hollow. When the passion for helping others turns into exhaustion, the potential for despair heightens.
The fear of being judged keeps many doctors from seeking help, creating a culture that conceals rather than addresses mental health struggles. The JAMA Network found that around 40% of physicians feel uncomfortable reaching out for support due to the potential repercussions on their careers. This stigma only adds to the weight they carry daily.
Unfortunately, easy access to medications and tools that can foster unhealthy outcomes plays a troubling role in this epidemic. The tragic death of Dr. Lorna Breen during the COVID-19 pandemic serves as a heartbreaking reminder of how swiftly despair can take hold.
A lack of mental health resources leaves many healthcare professionals feeling unsupported, trapped in a system that ignores their needs. Only 29% of physicians believe their workplace offers sufficient mental health resources, underscoring a dire need for institutional support.
The relentless pursuit of excellence can be a double-edged sword for doctors. The high standards set by training programs and society can create a breeding ground for feelings of inadequacy, making it hard for them to acknowledge their vulnerability.
Witnessing suffering on a daily basis can lead to emotional burnout, particularly for those who have faced personal loss. Healthcare professionals who deal with addiction—either through their work or personal experiences—often carry heavy emotional burdens, heightening their risk of psychological crises.
With demanding schedules and endless responsibilities, many doctors report feeling socially isolated. According to the Physicians Foundation, nearly half express a lack of close relationships, which can aggravate feelings of loneliness and depression in times of need.
The Writing on the Wall: Insights from Suicide Notes
Analyzing suicide notes left by doctors often reveals profound sadness and desperation. Time and again, the words reflect feelings of inadequacy, burden, and an overwhelming sense of failure. One heart-wrenching example is Dr. Julie A. Morrow’s note, where she candidly discussed the suffocating pressure of being a physician while battling her own depression.
These notes serve as powerful indicators of a larger issue in healthcare—the need for more open dialogues about mental health. By sharing insights from these tragic instances, we can cultivate a culture that prioritizes well-being and recognizes the silent suffering experienced by many.
Addressing the Side Effects of a Broken System
The ramifications of suicide by doctors go beyond those lost; they affect the entire healthcare structure. The repercussions extend into hospitals, where the remaining staff may endure what resembles PTSD symptoms, impacting their work and personal lives.
To combat this, healthcare institutions must step up. Implementing comprehensive wellness programs, providing adequate mental health resources, and creating safe channels for reporting mental health struggles can foster a supportive environment. It’s crucial to shift the culture from one that stigmatizes mental health to one that encourages open dialogues about emotional well-being.
Moving Forward: Innovative Solutions for a Healthier Workforce
Innovative solutions exist to reshape mental health resources for physicians. Programs that pair seasoned doctors with newcomers offer mentorship opportunities that provide oversight and emotional support. Peer-support networks can pave the way for candid discussions around mental health, normalizing vulnerability and connection.
Furthermore, increasing accessibility to mental health services can empower healthcare workers to seek help more freely. By actively working to dismantle the stigma surrounding mental illness, we can encourage more open conversations and, ultimately, save lives.
Breaking the Silence: A Call to Action
Examining the tragic reality of suicide by doctors sparks essential conversations on mental health within the medical field. It’s crucial for healthcare systems, policy-makers, and society to rally behind efforts that prioritize mental health support and foster resilience in our communities.
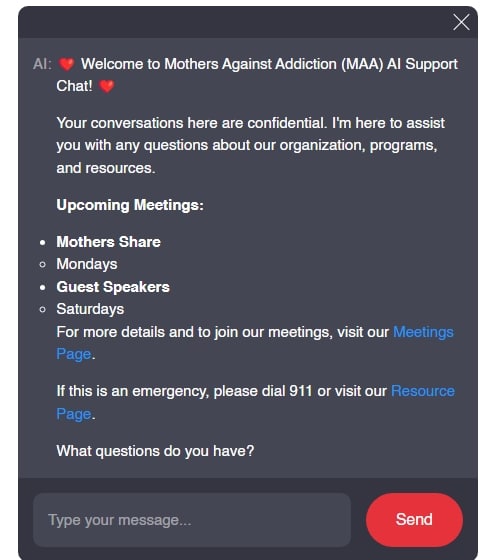
By addressing this silent epidemic, we not only honor the lives lost but also work to forge a healthier future for those who devote their lives to caring for others. If you or someone you know is struggling with addiction, fear, or loss, consider seeking help. Organizations like Mothers Against Addiction provide resources and community support for parents grappling with the heartbreak of addiction and its consequences. Together, we can break the silence, lift each other up, and move toward healing.
Suicide by Doctors: Unseen Struggles in Healthcare
The Hidden Crisis Among Healthcare Workers
Suicide by doctors isn’t just a shocking headline; it reflects a troubling trend that can no longer be ignored. Research indicates that physicians have a higher risk of suicide compared to the general population. Factors like long hours, high stress, and emotional strain contribute significantly to this crisis. Interestingly, just as many new mothers face the risk of postpartum issues, doctors too are vulnerable to mental health challenges that often go unaddressed. Understanding the Signs Of postpartum depression can help create a supportive environment—not just for parents but also for healthcare professionals who may feel alone in their struggles.
Impact of Stress and Burnout
It’s easy to see how the demanding nature of a medical career leads to burnout, often pushing doctors to the brink. Like an athlete perfecting their form, healthcare workers need to pay attention to their mental wellbeing just as they would a barbell front squat. Stress, when left unchecked, can spiral into depression and anxiety, amplifying the risk of suicide by doctors. We might not always recognize how deeply these pressures weigh on them. For instance, managing a personality disorder not only affects the individual but can have far-reaching consequences in their professional and personal life. Taking a personality disorder test might be a useful first step toward addressing these challenges.
Cultural Influences and Stigma
The stigma surrounding mental health in the medical profession is like a heavy fog, obscuring the path to seeking help. Stories of resilience, such as that of Rae Carruth, remind us of the dire emotional fallout that can ensue if someone doesn’t reach out for support. In a society where vulnerability is often seen as a weakness, it can be tough for doctors to admit they’re struggling. Whether it’s through openly discussing addiction—like asking, can You get addicted To weed ?—or( seeking assistance from systems like the Ohio board Of Pharmacy for resources, breaking down these barriers is vital.
In the thick of sweeping changes in healthcare and societal expectations, addressing the issue of suicide by doctors is paramount. It’s about more than just supporting doctors—it’s about creating a culture where healthcare workers can thrive. After all, we want these professionals to be able to focus on saving lives, not just on pizza breaks and discussions about The pizza edition. If we can foster open conversations around mental health, we stand a better chance of preventing tragedies and ensuring that those who care for us are also taken care of. So let’s not wait for a wake-up call. Just as your local Miniso store has all sorts of goodies to care for yourself, reaching out for emotional support is just as essential!